The vein of Giacomini: an in-depth review of its anatomy, hemodynamics, and treatment alternatives
Agnieszka Nowak-Tarnawska, MD
Department of Angiology and
Vascular Surgery, University
Hospital Central de la Cruz Roja,
Madrid, Spain; Associate Professor,
Faculty of Medicine, University
Alfonso X el Sabio, Madrid, Spain
Lourdes Reina-Gutierrez, MD
Head of the Department of
Angiology and Vascular Surgery,
University Hospital Central de la
Cruz Roja, Madrid, Spain; Associate
Professor, Faculty of Medicine,
University Alfonso X el Sabio,
Madrid, Spain
ABSTRACT
The vein known as the “vein of Giacomini” or “Giacomini vein” is part of the venous network of the lower limb and is involved in the drainage of the posterior part of the thigh. This vein owes its name to the Italian professor of anatomy who was the first to describe it in 1873. Giacomini observed that this vein acts as a proximal extension of the small saphenous vein and may follow multiple anatomical courses. Moreover, its most intriguing feature is that it can have more than 1 hemodynamic pattern depending on its valve arrangement and, most interesting, it leads to 2 different types of reflux when this vein becomes incompetent. Minimally invasive surgical options for this vein insufficiency include thermal ablation or ultrasound-guided foam sclerotherapy. These options allow for focused treatment of the leak point for both types of reflux. This article reviews the anatomy of the Giacomini vein, its hemodynamics and reflux variations, and the current treatment modalities for Giacomini-vein-related venous insufficiency.
Definition
The saphenous system, located within the saphenous compartment delimited by the superficial fascia and the muscular fascia, deserves special attention as it is not a classic “superficial” venous system.1 This compartment contains the great saphenous vein (GSV), the small saphenous vein (SSV), their accessories, and the “vein of Giacomini” or “Giacomini vein” (GV).
The GV, which is essentially a proximal extension of the SSV into the thigh, can have several anatomical variations. It may have various proximal endings, including the common variation of joining the GSV, albeit in some cases it may not be present at all.
Historical background
Carlo Giacomini, who studied the anatomy of lower-limb veins, observed the frequent presence of a thigh extension (TE) of the SSV. He described it in 1873 after dissecting 51 lower limbs. In his study, some type of TE of the SSV was present in 94% of the legs, with different anatomical patterns.2
Georgiev2 summarized those findings and grouped them into types, such as an intersaphenous anastomotic branch to the GSV, branches terminating as a vein of the small ischiatic nerve, branches communicating with perforators of the thigh, or branches ending in the thigh muscles (Figure 1). These types may or may not coincide with the presence of a saphenopopliteal junction (SPJ).
Georgiev also noted the contribution of Giacomini in determining that the presence of different proximal terminations of the SSV was a normal, most common condition and recognizing that the TE and the SSV, due to their fascial location, were parts of the same vein.
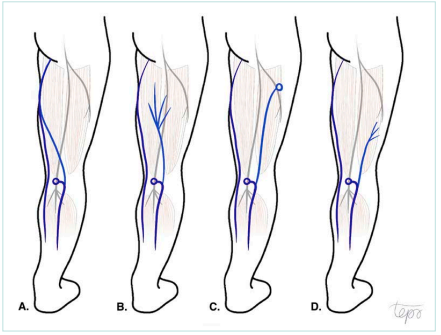
Figure 1. Schematic representation of Giacomini’s findings. A) An intersaphenous anastomotic branch to the great saphenous vein (GSV). B) Termination as a vein of the small ischiatic nerve. C) Branches communicating with perforators of the thigh. D) Branches ending in the thigh muscles. These types may or may not coincide with the presence of a saphenopopliteal junction. Drawn by Topo (IG: @artsy.topo) for the author’s personal collection.
Anatomy and nomenclature
After Giacomini, there have been many subsequent anatomic postmortem studies that have confirmed Giacomini’s findings, albeit with varying results until the advent of ultrasound imaging.
Venous ultrasound plays a crucial role in visualizing the TE. The TE appears as an ascending branch of the SSV in the lower thigh, situated in the interfascial layer between the semitendinosus and semimembranosus muscles medially and the long head of the biceps laterally (Figure 2). More proximally, it can penetrate deeper layers to join the deep venous system or end laterally in a muscle or have a circumflex course toward the GSV.

Figure 2. A transverse ultrasound image of the thigh extension at the lower thigh (blue arrow) in the interfascial layer between the semitendinosus and semimembranosus muscles medially (on the left) and the long head of the biceps laterally (on the right). Image from the collection of the Vascular Department at Cruz Roja University Hospital.
Recent studies using duplex ultrasound scanning (DUS) have reported the presence of the TE in 63.2%,34 and up to 70.4%5 of cases. According to Giacomini’s research, the TE of the SSV can differ anatomically between individuals. However, the most frequent variation is the anastomotic connection between the SSV and GSV (72%).2 This anastomotic connection, as observed by Giacomini, was the most frequent variation in Delis’ ultrasound study (49.5%).5 The Vascular Surgery Department in Cruz Roja Hospital in Madrid conducted an ultrasound observational study in 2022 that revealed the TE presence in 90% of 100 venous ultrasound explorations of lower limbs, and 48% of these showed an intersaphenous anastomotic variant.6,7
Considering the different anatomical courses that TE can adopt, the International Union of Phlebology (UIP) published a consensus on using different names based on the anatomy of the vein. The vein that ascends between the biceps femoris and semimembranosus muscles and ends in either deep or superficial veins of the thigh via perforators or via venous branches is referred to as the TE of the SSV.8 The one that connects to the GSV through the posterior thigh circumflex vein is referred to as the GV.8
Hemodynamic features
There is an additional discovery by Giacomini concerning these veins.
He discovered that they can have one of 2 possible and opposite valve arrangements that enable either normal upward or normal downward flow.
The intersaphenous GV is a classic example of the valve arrangement that permits upward blood flow. Some other proximal projections of the SSV may also exhibit this pattern, particularly when the SPJ is not present. Figure 3 shows a schematic representation of an upward-flowing valve arrangement.
On the other hand, the TEs that work as tributaries to the SPJ, such as the TE that terminates as muscular thigh branches, have valves that work in reverse in order to facilitate downward blood flow into the popliteal vein.2 Figure 4 shows a schematic representation of a downward-flowing valve arrangement.
Veins with normal upward blood flow may become incompetent due to a proximal leak point, eg, the GSV, proximal perforators, or pelvic connections. This leads to a conventional gravitational reflux, which is observed as diastolic reflux when the calf muscles are released after the squeezing maneuver (Figure 5). This reflux can end at the SPJ, draining into the popliteal vein, or may continue toward the SSV axis.
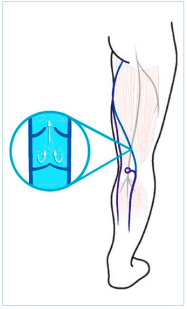
Figure 3. Schematic representation of an upward-flow-allowing valve arrangement. Drawn by Topo (IG: @artsy. topo) for the author’s personal collection
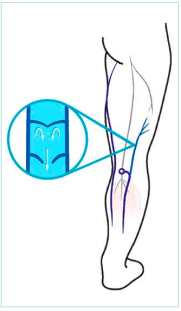
Figure 4. Schematic representation of a downward-flow-allowing valve arrangement. Drawn by Topo (IG: @artsy. topo) for the author’s personal collection.
Veins with normal downward blood flow have valves that prevent the upward flow from the SPJ. Therefore, in cases of valvular malfunction and vein incompetence, a completely different reflux is observed: an upward reflux becomes noticeable (paradoxical antigravitational reflux).
The upward reflux may be difficult to detect with a duplex examination due to its paradoxical pattern and occasional low flow. It is considered paradoxical because during muscular diastole the flow goes in the same upward direction as the manually induced systolic flow (Figure 6).
It may seem contradictory to consider an upward flow as pathological. However, in a duplex exam, the absence of venous flow during muscular diastole is normal, whereas both downward and upward flows lasting over 0.5 seconds during the diastolic phase should be considered pathological. For this reason, upward flow during diastole is a reflux that arises from a distal leak point such as the SPJ.2,9
The information about these 2 possible flow and reflux patterns is important to keep in mind during clinical and duplex examinations in order to anticipate identifying them.
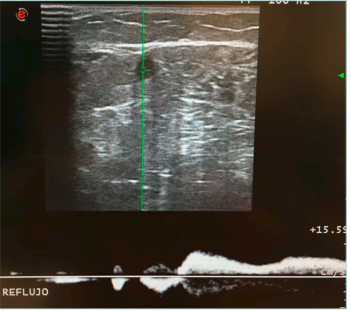
Figure 5. A transverse duplex image of the thigh extension at the lower thigh, with gravitational diastolic reflux that is opposite to the manually induced systolic flow (squeezing maneuver). Image from the collection of the Vascular Department at Cruz Roja University Hospital.
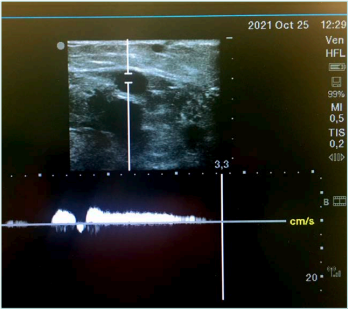
Figure 6. A transverse duplex image of the thigh extension at the lower thigh, with paradoxical diastolic reflux that goes in the same direction as the manually induced systolic flow (squeezing maneuver). Image from the collection of the Vascular Department at Cruz Roja University Hospital.
Giacomini vein and thigh extension reflux prevalence
DUS is an ideal method for examining the pattern and magnitude of venous reflux.
Studies vary in methodology but provide insight into the prevalence of GV insufficiency.
Georgiev et al found GV reflux in 6.2% of 1226 limbs with GSV or SSV insufficiency. It corresponded to paradoxical reflux in 30% of cases.2 Delis et al5 observed GV reflux in 3.3% of 301 limbs with suspected chronic venous disease; Labropoulos et al10 found it in 17.4% of 226 limbs with isolated reflux in the SSV system; and Escribano et al9 detected GV paradoxical reflux in 1.1% of 1350 limbs with varicose veins. In our department’s study at Cruz Roja Hospital, 5% of 100 examined limbs showed GV or TE insufficiency. Out of that, 1% had paradoxical reflux.6,7
Considering these findings, although somewhat varied, they confirm the potential for incompetence in veins within the Giacomini system and that they can exhibit both typical/ gravitational and paradoxical/antigravitational reflux.
Treatment options reports
The popliteal fossa, where Giacomini-system veins rise, is a complex anatomical area.
It can be challenging to perform surgical treatment due to the complex neurovascular relationships and anatomical variability of the venous structures.11
In view of this, a simple removal of superficial varicose branches, without surgical dissection of the insufficient Giacomini vein could be done as a single procedure.
Regarding this option, Escribano et al9 noticed a significant number of varicose veins recurrences (57%) after a 12-month follow-up. Thus, he suggested a CHIVA procedure (CHIVA—a French acronym for Conservatrice Hémodynamique de l’Insuffisance Veineuse en Ambulatoire) that involves surgically interrupting an insufficient GV (with paradoxical reflux) at the junction with the SSV as a more effective treatment, with only 13% of recurrences after a 12-month follow-up.9
More recently, endovascular treatments have emerged as convenient, effective, and secure options for treatment, especially for incompetent saphenous veins. In the same way, reports have emerged regarding endothermal laser treatment for GV insufficiency.
Bush et al12 used a combination of endolaser thermal ablation and ultrasound-guided foam sclerotherapy (UGFS) to treat 14 patients who had varicose veins due to TE insufficiency (including both TE and GV variants). The laser fiber was advanced proximally from the SSV as far as possible within the GV or TE for thermal ablation. Foam sclerotherapy was necessary for the proximal angulated or subcutaneous portions of the GV or TE, as well as for the posterior thigh perforators. The author did not report complications such as sural nerve damage or deep vein thrombosis nor were there any recurrences after 2 years of follow-up.
Theivacumar et al13 documented 2 cases of endolaser ablation of the GSV as a treatment of the paradoxical reflux of the GV. This approach served as a solution for reflux transmitted from the SPJ to the GSV through the intersaphenous connection. The ablation was performed on the GSV by puncturing it in the calf, from behind to above the point where the GSV joins the GV. He stated that the SPJ and the GV regained competency within 12 weeks. The reasoning behind this approach is that the SPJ is not responsible for this type of reflux. It is not a common approach, and an extensive follow up should be done to rule out recurring disease.
Park el al14 reported endolaser ablation of 18 incompetent GV (16 with gravitational reflux and 2 with anterograde “paradoxical” reflux), utilizing the SSV or GV as the primary access point, but employing the proximal GSV as a secondary option if needed. The observed endolaser-related adverse effects included bruising (56%), which had resolved by the 1-month follow-up, and tightness or pain at the treatment site (12.7%), both of which improved or resolved by 6 months. The author acknowledges the study’s limitations, including the loss of 66.7% of patients at the 12-month follow-up and the absence of anatomical details regarding the incompetent GV. However, he concluded that endolaser ablation provided a safe, effective, and technically successful solution for GV insufficiency.
The Guzelmansur et al15 retrospective study represents the largest group of patients (32 patients, 39 limbs) treated for GV insufficiency through endovenous ablation. The authors treated both the intersaphenous GV and the TE but did not identify the reflux type as conventional or paradoxical. Endolaser thermal ablation was used for treating straight incompetent GV (29 limbs), whereas UGFS was used on tortuous veins that were unfit for endolaser treatment (10 limbs). Likewise, endolaser therapy was employed for treating coexisting incompetent saphenous trunks. The authors did not report any complications, only transient discomforts. With a maximal follow-up up to 12 months, there was complete success in the endolaser group and only 1 recanalization in the UGFS group.
Targeted endovenous treatment of varicose disease associated with GV insufficiency (any type of reflux) demonstrated safety and efficacy in a study by Atasoy et al16 involving 17 patients. Straight GVs were treated with endolaser and tortuous GVs with UGFS (in 3 cases). As a treatment focused on reflux sources, it allowed the unnecessary ablation of healthy saphenous veins to be avoided.
Discussion
The presence of different proximal endings of the SSV that extend toward the thigh is a common and prevalent condition known as the TE of the SSV. Due to their contiguous location, both the TE and the SSV can be considered components of the same vein.
The most common anatomical variation of the TE is the intersaphenous anastomotic branch, also referred to as the Giacomini vein (GV).
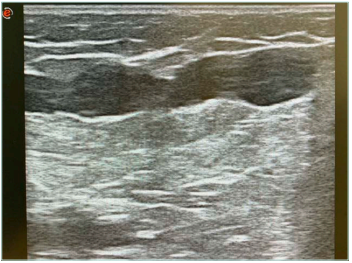
Figure 7. A longitudinal ultrasound view of a tortuous thigh extension located in the middle third of the thigh. Image from the collection of the Vascular Department at Cruz Roja University Hospital.
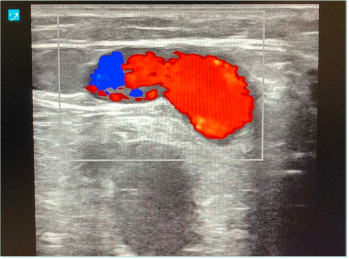
Figure 8. A transverse duplex image of a tortuous thigh extension located in the distal third of the thigh. Image from the collection of the Vascular Department at Cruz Roja University Hospital.
Although the GV is a connection between 2 subfascial saphenous veins, it frequently has 3 segments, with the middle segment located superficially within the subcutaneous tissue.2,4,9 On the other hand, when the GV is incompetent, it often becomes tortuous and angulated. These anatomical features are important to consider when deciding on treatment options (Figures 7 and 8).
Another important consideration for treatment decisions is these veins’ ability to exhibit 2 possible types of reflux, which are opposite to each other, due to 2 distinct and opposite valve arrangements. As a result, GV insufficiency can cause either a conventional, gravitational reflux or a paradoxical, antigravitational reflux.
It is important to think about the likelihood of paradoxical reflux in order to spot it in an ultrasound exam. By extension, reflux identification enables the reflux-oriented and therefore more effective treatment.
Based on current recommendations, the reflux source should be treated using a minimally invasive technique.
There is currently no established standard treatment for varicose vein disease associated with GV insufficiency. Therefore, extrapolating the recommendations for saphenous vein treatment may be an option.
The European Society for Vascular Surgery (ESVS) clinical practice guidelines17 on the management of chronic venous disease (CVD) of the lower limbs recommend endovenous thermal ablation as the first-choice technique for treating the GSV and SSV insufficiency, whereas UGFS can be considered for trunks with a diameter less than 6 mm. On the other hand, UGFS “is the technique of choice for anatomical configurations that make endovenous cannulation or advancing the ablation device challenging and is suitable for treating tortuous varicose veins.”17
So, although thermal ablation is the preferred technique for saphenous trunks, it has certain drawbacks when used for GV insufficiency; for example, due to the frequently tortuous or partially subcutaneous course of this vein. In fact, only 1 of the aforementioned authors14 reported a completely endolaser-based thermal ablation of GV insufficiency, although it is not possible to know the anatomical characteristics of the veins in this study. The remaining authors considered it necessary to use a combined treatment approach, using endolaser for straight vein segments and UGFS for elongated ones.
On the other hand, the possibility of thermal damage to adjacent nerves is a logical concern, especially in the popliteal fossa, a high-risk area due to its numerous nerves and variable anatomy. This includes the possibility of anatomical proximity between the GV and the sciatic bifurcation, as well as the tibial and peroneal nerves.18 In Figure 9, imaging shows the tibial nerve located near the TE vein in the distal part of the thigh. Regarding the GV in particular, it has its neural companion in the thigh, the posterior femoral cutaneous nerve (Figure 10).
According to Uhl and Gillot’s theory of “angio-guiding” nerves that determine the venous development of the embryo, the posterior femoral cutaneous nerve corresponds to the former postaxial nerve that guides the TE of the SSV.1 The posterior femoral cutaneous nerve is a sensory nerve, and its neuropathy causes pain in the inferior gluteal area and the posterior part of the thigh.
Of the published studies of thermal ablation for GV insufficiency, Park et al14 reported mild transient symptoms of neuronal distress (in 12.67% of cases). It is important to note that in this study, the entire length of the GV was treated solely with thermal ablation, without the use of foam sclerotherapy.

Figure 9. Tibial nerve located near the thigh extension vein in the distal part of the thigh, indicated by 2 white crosses. Image from the collection of the Vascular Department at Cruz Roja University Hospital.

Figure 10. The white arrow indicates the posterior femoral cutaneous nerve located near the thigh extension vein in the middle/upper part of the thigh. Image from the collection of the Vascular Department at Cruz Roja University Hospital.
In the field of Peripheral Nerve Surgery and Research, there is a report of a common peroneal nerve injury following endolaser thermal ablation of the GV.18 The article mentions an endovenous laser treatment from 10 centimeters below the knee to 20 centimeters above the knee, delivering 4010 J at 14W. The patient experienced immediate postoperative numbness and was unable to evert their ankle. Electromyogram demonstrated a severe peroneal neuropathy. There was no motor or sensory recovery after 9 months of follow-up. In conclusion, the authors emphasize the importance of precise preoperative ultrasound-guided mapping of venous and neural structures. The relative anatomic relationship between these structures should be the guiding principle in selecting the level of venous thermal ablation.18
In summary, data on thermal neuropathy after GV ablation are still too limited to draw definitive conclusions.
As previously mentioned, the ESVS guidelines highlight UGFS as a recommended treatment option for anatomically challenging and tortuous venous configurations, which frequently happen in the case of the GV. The Vascular Surgery Department in Cruz Roja Hospital considers UGFS as the preferred approach for treating GV insufficiency. In our experience, UGFS can be used as a single technique for any type of GV or TE, regardless of the complexity of its anatomical course or depth. In addition, UGFS does not endanger nerve integrity.
To implement the leak-point–focused strategy while performing UGFS, it is crucial to conduct a comprehensive duplex mapping of GV insufficiency to determine the type of reflux. This allows for a hemodynamic treatment, as the leak point is targeted first.
In the case of varicose TE or GV caused by upward reflux (paradoxical antigravitational reflux), the initial puncture for foam injection is performed near the SPJ, which corresponds to the leak point. Then, the next venous segment not filled with foam is punctured and filled, and the treatment is completed from a distal to a proximal part of the thigh. See Figures 11-13.
To treat downward reflux (conventional gravitational reflux), staged injections should be administered from the upper part of the thigh toward the calf, along the targeted vein.

Figure 11. Patient with varicose veins caused by upward paradoxical reflux of the thigh extension vein. Picture before treatment. Image from the collection of the Vascular Department at Cruz Roja University Hospital.

Figure 12. Ultrasound-guided foam sclerotherapy is used to treat the incompetent thigh extension vein. The first injection is administered near the saphenopopliteal junction. Subsequent injection involves filling the next unfilled segment with foam, moving toward the proximal part of the thigh. Image from the collection of the Vascular Department at Cruz Roja University Hospital.
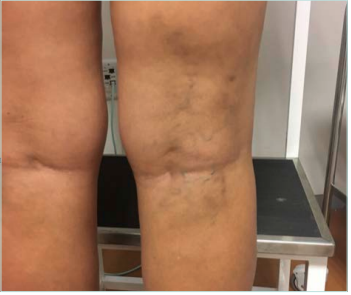
Figure 13. Six months after 1 session of ultrasound-guided foam sclerotherapy of the incompetent thigh extension vein. Image from the collection of the Vascular Department at Cruz Roja University Hospital.
Conclusions
The so-called “Giacomini vein” (GV) refers to a range of anatomical courses of the TE of the SSV that can vary anatomically between individuals. They are commonly found in the human lower limb and the most frequent variation is the anastomotic connection between the SSV and GSV, which should actually be referred to as the GV.
Aside from exhibiting anatomical variability, these veins can have one of 2 possible (and opposite) valve arrangements, depending on their drainage function. Due to this feature, when the vein becomes insufficient, it can result in one of 2 types of reflux that are opposite to each other. During duplex examinations, it is important to keep in mind the 2 possible flow and reflux patterns, especially the likelihood of paradoxical (or upward) reflux.
For GV and TE venous insufficiency, minimally invasive surgical options include thermal ablation or UGFS. These options enable targeted treatment of the leak point in both upward- and downward-directed reflux. In cases of endothermal ablation, a thorough preoperative ultrasound examination of venous and neural relationships is crucial to minimize the risk of thermal nerve injury.
UGFS is a suitable treatment option for anatomically challenging varicose veins, which are particularly common within the GV system. Additionally, it is a nerve-safe technique.

CORRESPONDING AUTHOR
Agnieszka Nowak, MD
Servicio de Angiología y Cirugía Vascular,
Avda. Reina Victoria, 24 (consulta planta
-1), 28003 Madrid, Spain
email: doctoranowak@gmail.com
References
1. Uhl JF, Gillot C. Anatomy and embryology of the small saphenous vein: nerve relationships and implications for treatment. Phlebology. 2013;28(1):4-15. doi:10.1258/phleb.2012.012j08.
2. Georgiev M, Myers KA, Belcaro G. The thigh extension of the lesser saphenous vein: from Giacomini’s observations to ultrasound scan imaging. J Vasc Surg. 2003;37(3):558-563. doi:10.1067/ mva.2003.77.
3. Engel AF, Davies G, Keeman JN, von Dorp TA. Colour flow imaging of the normal short saphenous vein. Eur J Vasc Surg. 1994;8(2):179-181. doi:10.1016/s0950- 821x(05)80456-6.
4. Caggiati A. Fascial relationships of the short saphenous vein. J Vasc Surg. 2001;34(2):241-246. doi:10.1067/ mva.2001.116972.
5. Delis KT, Knaggs AL, Khodabakhsh P. Prevalence, anatomic patterns, valvular competence, and clinical significance of the Giacomini vein. J Vasc Surg. 2004;40(6):1174-1183. doi:10.1016/j. jvs.2004.09.019.
6. Nowak A. Sclerotherapy as a reflux focused and selective treatment of Giacomini vein insufficiency. Presented at: 80th Congress of Societe Francaise de Phlebologie; December 1, 2022; Paris, France.
7. Nowak A, Reina L. Prevalence, anatomics and hemodynamics of Giacomini’s vein variants in a sample of 100 venous doppler ultrasound exams. Presented at: 30 Congreso Nacional del Capítulo Español de Flebología y Linfología de la SEACV; April 28, 2023; Vigo, Spain.
8. Cavezzi A, Labropoulos N, Partsch H, et al. Duplex ultrasound investigation of the veins in chronic venous disease of the lower limbs–UIP consensus document. Part II. Anatomy. Eur J Vasc Endovasc Surg. 2006;31(3):288-299. doi:10.1016/j. ejvs.2005.07.020.
9. Escribano JM, Juan J, Bofill R, et al. Haemodynamic strategy for treatment of diastolic anterograde giacomini varicose veins. Eur J Vasc Endovasc Surg. 2005;30(1):96-101. doi:10.1016/j. ejvs.2005.03.001.
10. Labropoulos N, Giannoukas AD, Delis K, et al. The impact of isolated lesser saphenous vein system incompetence on clinical signs and symptoms of chronic venous disease. J Vasc Surg. 2000;32(5):954-960. doi:10.1067/mva.2000.110349.
11. O’Donnell TF, Iafrati MD. The small saphenous vein and other “neglected” veins of the popliteal fossa: a review. Phlebology. 2007;22(4):148-155. doi:10.1258/026835507781477172.
12. Bush RG, Hammond K. Treatment of incompetent vein of Giacomini (thigh extension branch). Ann Vasc Surg. 2007;21(2):245-248. doi:10.1016/j. avsg.2006.07.008.
13. Theivacumar NS, Dellagrammaticas D, Mavor AID, Gough MJ. Endovenous laser ablation (EVLA) of great saphenous vein to abolish “paradoxical reflux” in the Giacomini vein: a short report. Eur J Vasc Endovasc Surg. 2007;34(2):229-231. doi:10.1016/j.ejvs.2007.01.011.
14. Park SW, Lee SA, Hwang JJ, et al. Early results of endovenous ablation with a 980-nm diode laser for an incompetent vein of Giacomini. Korean J Radiol. 2011;12(4):481-486. doi:10.3348/ kjr.2011.12.4.481.
15. Guzelmansur I, Oguzkurt L, Koca N, Andic C, Gedikoglu M, Ozkan U. Endovenous laser ablation and sclerotherapy for incompetent vein of Giacomini. Phlebology. 2014;29(8):511-516. doi:10.1177/0268355513496552.
16. Atasoy MM, Gümüş B, Caymaz I, Oğuzkurt L. Targeted endovenous treatment of Giacomini vein insufficiency-associated varicose disease: considering the reflux patterns. Diagn Interv Radiol Ank Turk. 2014;20(6):481-486. doi:10.5152/ dir.2014.14148.
17. De Maeseneer MG, Kakkos SK, Aherne T, et al. Editor’s Choice – European Society for Vascular Surgery (ESVS) 2022 clinical practice guidelines on the management of chronic venous disease of the lower limbs. Eur J Vasc Endovasc Surg. 2022;63(2):184-267. doi:10.1016/j. ejvs.2021.12.024.
18. Shahid KR, Dellon AL, Amrami KK, Spinner RJ. Sciatic and peroneal nerve injuries after endovascular ablation of lower extremity varicosities: case reports and review of the literature. Ann Plast Surg. 2015;74(1):64. doi:10.1097/SAP.0000000000000193.
