The role of compression in the prevention of postthrombotic syndrome
Athanasios D. GIANNOUKAS
Department of Vascular Surgery, University
Hospital of Larissa, University of Thessaly Medical
School, Larissa, Greece.
ABSTRACT
The role of compression with or without early ambulation in patients with deep venous thrombosis (DVT) in the prevention of postthrombotic syndrome (PTS) has not been widely accepted in clinical practice. This article investigates the existing evidence regarding the effects of compression in the prevention of PTS, with or without early ambulation after proximal DVT.
Electronic and hand searching of the relevant literature was undertaken. Two systematic reviews and four randomized studies were identified. In these four studies there was lack of uniformity in reporting standards. In all but one study a clear benefit (48% risk reduction in the development of PTS) was shown by the use of compression with or without early ambulation, without any difference in respect of recurrent thromboembolic complications (DVT or pulmonary embolism). In one study the early symptomatic outcome was better with a combination of early ambulation plus compression.
Despite the lack of uniformity in reporting standards in the literature, compression with or without early ambulation appears to be associated with a decreased rate of PTS.
INTRODUCTION
Subcutaneous low-molecular-weight heparin (LMWH) has revolutionized the treatment of deep venous thrombosis (DVT), because it is at least as effective and safe as conventional unfractionated heparin,1-5 allowing outpatient treatment without the need for laboratory monitoring.3,5-7
There is lack of consensus regarding the definition of postthrombotic syndrome (PTS), and several scoring systems have been proposed to aid diagnosis. 8-10 Venous hypertension secondary to outflow obstruction or vein valve incompetence or both, and the condition of the calf muscle pump function, play an important role in the development of PTS.11-15.
Removable elastic bandages, inelastic adherent bandages, graduated compression elastic stockings, and intermittent compression pneumatic devices have all been used to reduce swelling by promoting acceleration of venous return and improving muscle pump function.16-20
This article investigates the evidence regarding the effects of compression on the prevention of PTS, with or without early ambulation after proximal DVT.
MATERIAL AND METHODS
A literature search was undertaken in MEDLINE from 1966 and EMBASE from 1980 using the terms DVT, elastic compression, compression, and PTS. Handsearching of the journals Phlebology (1990-2007), Journal of Thrombosis and Haemostasis (2003-2007), and the abstract books of the Annual Meetings of the European Venous Forum (2000-2007) and American Venous Forum (1989-2007) was undertaken. The references of relevant papers were also consulted.
Only systematic reviews and studies that had a randomized controlled design in the evaluation of any kind of compression treatment in patients with a proven proximal thrombosis (extended at least up to the popliteal vein) were considered.
RESULTS
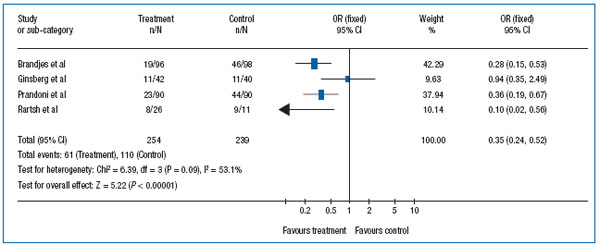
Four studies21-24 that met the inclusion criteria and two systematic reviews25,26 were identified. In all but one study22 compression was associated with beneficial effects in the prevention of PTS. The benefit conferred in each study separately and when all four studies were considered together was analyzed in a systematic review (Table I).26 This analysis showed that PTS developed in 24% (61/254) of patients in the compression group and in 46% (110/239) in the control group (x2= 25.36, P=0.0001; odds ratio, 0.37; 95% confidence interval [CI], 0.25-0.54; relative risk [RR], 0.52; 95% CI: 0.40-0.67; RR reduction,: 0.48; 95% CI, 0.33-0.60), with a 48% risk reduction because of the use of compression.
DISCUSSION
The diversity in standards of reporting PTS remains unresolved. The pain and swelling that patients experience during the acute phase of proximal DVT usually subside within two to twelve weeks as a result of various factors, including the lytic process of the thrombus, how fast the recanalization occurs, as well as the timing of the development of collateral flow.14,15 However symptoms similar to those of PTS, such as leg pain, aching, and swelling on standing, may persist despite the good compensation of the thrombotic process. Additionally, it should be acknowledged that not all patients develop PTS after proximal DVT.22 The devel- opment of true PTS is a consequence of venous hypertension secondary to venous valvular incompetence or occasionally to residual venous obstruction or to both.27-29 The adoption of the most recent CEAP classification10 in future studies may help overcome the problems in reporting PTS.
Another diversity found in the literature21-24 was in the type of compression and the timing of its application after the onset of DVT. The latter varied from immediately after the index event to three weeks. In one study22 the control group was also given elastic stockings one to two sizes too large, which still can exert some compression. Furthermore, the treatment group in this study22 was given elastic stockings that exerted a pressure of 20-30 mm Hg at the ankle. In two of the other studies,21,23 compression at the ankle was 30 to 40 mm Hg, and in the remaining study24 compression was offered either by combination of a firm inelastic bandage with Unna’s boot and a firm adhesive bandage or by thigh length compression stockings.
Nevertheless, all but one study22 demonstrated that compression offers significant benefit, with 48% risk reduction in PTS development. Additionally, early ambulation even at the acute phase of DVT combined with compression offered a more favorable symptomatic outcome compared with bed rest.30,31 This adds further to the perceived benefits of the treatment of DVT with LMWH by offering early symptomatic relief and improved well-being.
In conclusion, compression with or without early ambulation appears to be associated with a decreased rate of PTS without any increased risk of recurrent thromboembolism. However, because of the methodological defects in the relevant literature, a large, randomized, controlled trial is needed to prove these effects conclusively. Alternatively, if such study is questionable on ethical grounds a large observational study could be done instead.
Finally, future studies should address issues such as the optimal timing of elastic compression, the minimum duration that stockings must be worn after the episode of DVT, and the pressure required to optimize the beneficial effects.
REFERENCES
2. Lensing AW, Prins MH, Davidson BL, Hirsh J. Treatment of deep venous thrombosis with low-molecular-weight heparins. A meta-analysis. Arch Intern Med. 1995;155:601-607.
3. Levine M, Jent M, Hirsh J, et al. A comparison of low-molecular-weight heparin administered primarily at home with unfractionated heparin administered in the hospital for proximal deep-vein thrombosis. N Engl J Med. 1996;334:677- 681.
4. Wells PS, Kovacs MJ, Bormanis J, et al. Expanding eligibility for outpatient treatment of deep venous thrombosis and pulmonary embolism with low-molecularweight heparin: a comparison of patient self-injection with homecare injection. Arch Intern Med. 1998;158:1809-1812.
5. Buller, HR, Agnelli G, Hull RD, Hyers TM, Prins MH, Raskob GE. Antithrombotic therapy for venous thromboembolic disease. The Seventh ACCP Conference on Antithrombolytic and Thrombolytic Therapy. Chest. 2004;126(Suppl):401S- 428S.
6. No authors listed. ASHP Therapeutic Position Statement on the Use of Low- Molecular-Weight Heparins for Adult Outpatient Treatment of Acute Deep-Vein Thrombosis. Am J Health Syst Pharm. 2004;61:1950-1955.
7. Koopman MMW, Prandoni P, Piovella F, et al. Treatment of venous thrombosis with intravenous unfractionated heparin administered in the hospital as compared with subcutaneous low-molecular-weight heparin administered at home. The Tasman Study Group. N Engl J Med. 1996;334:682- 687.
8. Porter JM, Moneta GL. Reporting standards in venous disease: an update. International Consensus Committee on Chronic Venous Disease. J Vasc Surg. 1995;21:635-645.
9. No authors listed. Classification and grading of chronic venous disease in the lower limbs. A consensus statement. Ad Hoc Committee, American Venous Forum. J Cardiovasc Surg. 1997;38:437-441.
10. Eklof B, Rutherford RB, Bergan JJ, et al. American Venous Forum International Ad Hoc Committee for revision of the CEAP Classification. Revision of the CEAP classification for chronic venous disorders: consensus statement. J Vasc Surg. 2004;40:1248-1252.
11. Prandoni P, Lensing AW, Cogo A, et al. The long-term clinical course of acute deep venous thrombosis. Ann Intern Med. 1996;125:1-7.
12. Christopoulos D, Nicolaides AN, Cook A, Irvine A, Galloway JM, Wilkinson A. Pathogenesis of venous ulceration in relation to the calf muscle pump function. Surgery. 1989;106:829-835.
13. Haenen JH, Janssen MC, Wollersheim H, et al. The development of post-thrombotic syndrome in relationship to venous reflux and calf muscle pump dysfunction at 2 years after the onset of deep venous thrombosis. J Vasc Surg. 2002;35:1184- 1189.
14. Meissner MH, Zierler BK, Bergelin RO, Chandler WL, Strandness DE Jr. Coagulation, fibrinolysis, and recanalization after acute deep venous thrombosis. J Vasc Surg. 2002;35:278-285.
15. Killewich LA, Bedford GR, Beach KW, Strandness DE Jr. Spontaneous lysis of deep vein thrombi: a rate and outcome. J Vasc Surg. 1989;9:89-97.
16. Partsch H. Compression therapy of the legs. A review. J Dermatol Surg Oncol. 1991;17:799-805.
17. Partsch H. Do we need firm compression stockings exerting high pressure? VASA 1984;13:52-57.
18. Brakkee AJM, Kuiper JP. The influence of compressive stockings on the haemodynamics in the lower extremities. Phlebology. 1988;3:147-153.
19. Neumann HAM, Tazelaar DJ. Compression therapy. In: Bergan JJ, Golman MP, eds. Varicose vein and telangiectasias. Diagnosis and treatment. 1st ed. St. Louis, Mo: Quality Medical Publishing Inc; 1993:103-122.
20. Kakkos SK, Szendro G, Griffin M, Sabetai M, Nicolaides AN. Improved hemodynamic effectiveness and associated clinical correlations of a new intermittent pneumatic compression system in patients with chronic venous insufficiency. J Vasc Surg. 2001;34:915-922.
21. Brandjes DPM, Buller HR, Heijboer H, et al. Randomised trial of effect of compression stockings in patients with symptomatic proximal-vein thrombosis. Lancet. 1997;349:759-762.
22. Ginsberg JS, Hirsh J, Julian J, et al. Prevention and treatment of postphlebitic syndrome: results of a 3-part study. Arch Intern Med. 2001;161:2105-2109.
23. Prandoni P, Lensing AWA, Prins MH, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome. Ann Intern Med. 2004;141:249-256.
24. Partsch H, Kaulich M, Mayer W. Immediate mobilisation in acute vein thrombosis reduces post-thrombotic syndrome. Int Angiol. 2004;23:206-212.
25. Kolbach DN, Sandbrink MWC, Hamulyak K, Neumann HAM, Prins MH. Nonpharmaceutical measures from prevention of post-thrombotic syndrome. The Cochrane Database of Systematic Review 2003, Issue 3, Art. No: CD004174.pub2.DOI:10.1002/14651858. CD004174pub2.
26. Giannoukas AD, Labropoulos N, Michaels JA. Compression with or without early ambulation in the prevention of postthrombotic syndrome: A systematic review. Eur J Vasc Endovasc Surg. 2006;32:217-221.
27. Van Haarst EP, Liasis N, Van Ramshorst B, Moll FL. The development of valvular incompetence after deep vein thrombosis: a 7 year follow-up study with duplex scanning. Eur J Vasc Endovasc Surg. 1996;12:295-299.
28. Strandness DE Jr, Langlois Y, Cramer M, Randlett A, Thiele BL. Long-term sequelae of acute venous thrombosis. JAMA. 1983;250:1289-1292.
29. Markel A, Manzo RA, Bergelin RO, Strandness DE Jr. Valvular reflux after deep vein thrombosis: incidence and time of occurrence. J Vasc Surg. 1992;15:377- 382.
30. Partsch H, Blattler W. Compression and walking versus bed rest in the treatment of proximal deep venous thrombosis with low molecular weight heparin. J Vasc Surg. 2000;32:861-869.
31. Blattler W, Partsch H. Leg compression and ambulation is better than bed rest for the treatment of acute deep vein thrombosis. Int Angiol. 2003;22:393-400.
