Skin necrosis as a complication of compression in the treatment of venous disease and in prevention of venous thromboembolism
Chassieu, France
BACKGROUND
The main concern with compression treatment for chronic venous disease of the lower limb remains compliance, which is difficult to assess depending on the clinical status. Complications like skin allergic reaction and eczema,1 and nerve palsy,2 have been reported, but the most severe is skin necrosis in diabetics or patients with peripheral arterial disease of the lower limbs. There is a consensus for contraindicating compression in patients whose ankle/brachial index (ABI) is less than 0.6, but the arterial disease is not always identified. Diabetes also carries a potential risk of skin wound, but few data are available.
LITERATURE REVIEW
A literature search for skin necrosis related to compression identified several articles,3-6 including the Scottish survey.7 The aim of this survey was to review the experience of Scottish surgeons over the past five years concerning skin necrosis induced or aggravated by compression of the lower limb. All 154 consultants in general surgery asked to complete a questionnaire did so. One third of them reported at least one case of damage induced by compression, and 20% more than one. The replies are shown in Table I.
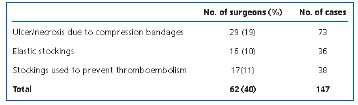
Table I. Compression damage.
Damage necessitated reconstructive arterial surgery in 7 cases and amputation in 12 (12/147= 8.2%). Other cases of amputation have been reported in the litterature (Figure 1).

Figure 1. High sustained pressure in a patient treated by compression bandages for a lateral leg ulcer with unrecognized occlusive arterial disease. The patient required a below knee amputation despite successful reconstructive surgery.
Image by courtesy of Prof H. Partsch, Vienna, Austria.
Our personal experience includes two diabetic patients who presented severe skin necrosis, related in both cases to stockings prescribed for thromboembolism prevention.
The Scottish survey does not, of course, give the prevalence of this complication, but the question of underand overreporting arises. Like the authors, I think the number was underestimated, for several reasons.
• The survey was retrospective and depended on recollection.
• The cause of this kind of damage often remains unrecognized.
• The survey was limited to consultant general surgeons, and excluded vascular surgeons, dermatologists, and angiologists.
• Eighty percent of patients with leg ulcers in the UK over this period were managed entirely in the community.

Figure 2. Bedsore at the popliteal fossa related to 2 panty hoses one pulled over the other worn 4 weeks after great saphenous stripping. Image by courtesy of Dr D. Creton, Nancy, France.

Figure 3. Heel bedsore related to 2 panty hoses one pulled over the other and worn day and night 6 weeks after great saphenous stripping. Image by courtesy of Dr D. Creton, Nancy, France.
CAUSE
Several causes of this complication can be identified:
• Compression is usually prescribed and applied by unspecialized therapists, and this may be harmful when using compression bandages.
• When compression is used to treat leg ulcers, between 20% and 30% of patients have impaired arterial blood supply in the ulcerated leg. This association is frequent in elderly patients; it has been estimated that up to 50% of patients over 80 years with leg ulceration also have a significant arterial disease.9
• Arterial investigation is not systematically undertaken before prescription of compression, and it is well known that clinical examination is unreliable or difficult in patients with edema or ulcerated legs.
RECOMMENDATIONS FOR ALLEVIATING THIS COMPLICATION
Ultrasound investigation including ABI measurement should be mandatory before the use of any kind of compression.
The manufacturer’s warnings are often neglected. We suggest highlighting the warning, as has been done on cigarette packs. In patients with an ABI <0.7, other treatment should be considered:
• prevention of thromboembolic risk by prescribing anticoagulation or mobilizing devices,
• improvement of chronic venous disease by drugs or interventional treatment according to the clinical status of the patient.
COMMENT BY PROFESSOR HUGO PARTSCH:
Beware of sustained compression!
An effective treatment always carries the risk of side effects. The margin between benefit and risk of compression therapy is determined by the pressure and the material of the compression device. Strong compression bandages with a resting pressure in the range of 40-60 mm Hg are successfully used in the treatment of venous leg ulcers, a disease that mainly involves elderly patients. Due to the reduction in edema the interface pressure of the bandages will drop instantly to a pressure range that is well tolerated in most cases. Unless distal pulses of good volume can be felt, Doppler pressures should be measured. If the arterial brachial pressure index is between 0.6 and 0.9 we recommend bandages with reduced compression (~20 mm Hg) and close surveillance of the patients. Inelastic short stretch bandages exert a massage effect during walking, which will reduce swelling and increase the blood flow. In a similar way intermittent pneumatic pressure machines have been shown to increase arterial blood flow and to reveal beneficial clinical effects even in patients with symptomatic arterial occlusive disease.
On the other hand, elastic material maintaining a constantly high resting pressure independent of body position exerts much lower pressure peaks during movement. Skin damage has been reported even with light thromboprophylactic stockings. Incorrect fitting and lack of daily surveillance seem to be the most important flaws in patient care in these cases.
Patient–related risk factors that have to be considered are not only age and arteriosclerosis but also sensory loss, eg, due to diabetic neuropathy. Sometimes the pain level associated with leg ulcers can be so severe that the occurrence of pressure sores caused by the compression device may not be recognized. To prevent postoperative compression complication after varicose vein surgery, the compression must be assessed by the surgeon and the patient informed that any postoperative persistent pain needs to be identified.
REFERENCES
2. Usmani N, Baxter KF, Sheehan-Dare R. Partially reversible common peroneal nerve palsy secondary to compression with four-layer bandaging in a chronic case of venous leg ulceration. Br J Dermatol. 2004;150:1224-1225.
3. Merret ND, Hanel KC. Ischaemic complications of graduated compression stockings in the treatment of deep venous thrombosis. Postgrad Med J. 1993;69:232-234. 4. Heath DL, Kent SJS, Johns DL, Young TW. Arterial thrombosis associated with graduated pressure antiembolic stockings. Br Med J. 1987;295:580.
5. Chan CL, Meyer FJ, Hay RJ, Burnand KG. Toe ulceration associated with compression bandaging: observational study. BMJ. 2001;323:1099.
6. Yaffe B, Shafir R. Complication with the elastic tubed net bandage. Orthoped Rev. 1986;15:553-554.
7. Callam MJ, Ruckley CV, Dale JJ, Harper DR. Hazards of compression treatment of the leg: an estimate from Scottish surgeons. Br Med J. 1987;295:1382.
8. Creton D. Cutaneous complications concerning the postsurgical dressing made with class 2 stockings. Phlébologie. 1998;51:363-364 (in French).
9. Callam MJ, Harper Dr, Dale JJ, Ruckley CV. Arterial disease in chronic leg ulceration: an underestimated hazard? Lothian and Forth Valley leg ulcer study. Br Med J. 1987;294:929.
