Popliteal vein entrapment: an unrecognized cause of failure in surgery for superficial venous insufficiency
Montpellier, France
SUMMARY
Positional compression of the popliteal vein syndrome, or popliteal vein entrapment, often goes unrecognized. For the last 5 years, we have systematically sought to detect this condition in cases where clinical signs suggest its presence. These are: edema related to position, cramps associated with prolonged standing, exertional pain together with cramps and swelling of the calf muscle in athletes, and asymmetry of the circumference of the anterior and posterior tibialis muscles.
The most frequent circumstances in which this condition is detected are:
• intensive muscle-building training in young women who practice highrisk sports;
• repeated recurrence of varicose veins in the area supplied by the short saphenous vein;
• recurrent sural vein thrombosis outside of any context of thrombophilia.
The diagnosis is confirmed by duplex scanning investigation with active and passive maneuvers, whose aim is to detect the position that triggers this condition. Imaging methods supplement the workup: dynamic venography, and dynamic MRI.
Surgery eliminates the compression at the cost of a relatively long incision to allow investigation of the vein along its entire length. A repeat check by perioperative maneuvers, possibly aided by electrical stimulation, confirms that the vein has been entirely freed in all positions. We operated on 11 patients, with immediate good results. In two patients, a supplementary aponeurotomy had to be performed.
Being aware of possible popliteal vein compression provides an effective solution to offer patients who are disappointed by the recurrence of their venous disorder.
INTRODUCTION
Although popliteal artery entrapment is a well-defined anatomic entity, whose treatment has received a broad consensus of approval, extrinsic compression of the popliteal vein syndrome, more recently recognized,1 is rarely systematically sought.
Treatment of this condition is subject to differences in terms of methods and indications. Some authors have proposed the term “popliteal vein entrapment syndrome” to associate so-called “functional forms” and anatomical forms, observed more rarely.
We prefer to use the term “popliteal vein extrinsic positional obliteration syndrome” referring to the triggering position found in these two entities. We have observed this syndrome in young athletes. It then most often involves the effect of overly intensive or improperly balanced physical training.
However, the systematic search for positional compression, in certain cases of an incompetent short saphenous vein, has allowed us to diagnose popliteal vein compression as the origin of many varicose recurrences. These cases can help in providing relief to patients with a recurrence of varicose veins refractory to the usual therapies.
MATERIAL AND METHODS
Since 2001, the diagnosis of popliteal vein compression requiring surgical intervention has involved 11 patients in our center.
Variable circumstances of detection
• Repeated recurrence of varicose veins in the area supplied by the short saphenous vein: four cases;
• Rapid-onset edema or swelling of the calf muscle during exertion in a young athlete: three cases;
• Unilateral positional edema: two cases;
• Recurrent sural vein thrombosis without thrombocytopenia: two cases. The patients’ ages ranged from 19 to 47 years: mean age = 28.4 years.
Eight out of the 11 patients were women.
The clinical examination consisted of the following
• A systematized interview to look for symptoms suggestive of this condition: Exertional edema or after standing for a prolonged period;
– Nighttime cramps or cramps occurring after prolonged sitting;
– Lane’s sign: alternating weight-bearing of one lower limb on the other in the standing position;
– Calf pain after wearing shoes without heels;
– Heaviness in the legs without superficial or deep reflux.
• The examination measures the leg circumference to detect possible asymmetry found in 8 out of 11 cases (Figure 1). It records the existence of varices in the area supplied by the short saphenous vein.

Figure 1. Asymmetry of calf muscles: multiple varicose vein
recurrence.
• Ultrasonographic hemodynamic examinations were performed with Esaote Partner duplex scanning and Hokanson continous Doppler:
– Duplex scanning of the popliteal vein is done in the standing position, with normal weight-bearing on the ball of the foot, with the knee locked in extension. The transducer is placed high on the popliteal vein to detect compression by the gastrocnemius muscle.
– Duplex scanning of the popliteal vein with the patient in the prone position, with his or her feet extended over the examining table.
• Morphological workup: to look for dilatation of the sural veins, in particular the posterior tibial veins, suggesting a soleus syndrome.
• Looking for a decrease or abolition of the arterial signal of the posterior tibial artery at the ankle during forced flexion of the foot.
• Passive maneuvers of the foot in flexionextension, with the leg stretched against the thigh, with the transducer placed on the middle of the popliteal vein, and then on the upper part of the popliteal vein.
• Active maneuvers: of flexion of the foot against resistance to obtain optimum contraction of the calf muscles.
– Dynamic ascending venography was the main component of the diagnosis.
– Anterior and lateral views, with the leg at rest and then with flexion/extension of the foot; if necessary with the foot in weight-bearing position with the examing table tilted to 60, combined with varicography in cases of recurrent varicose veins. It was always performed in the surgeon’s presence (Figures 2 and 3).
– We did not use modern imaging methods, ie, angio-scanning and angio-NMR, because venography confirmed the diagnosis.
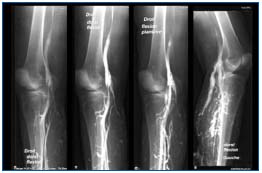
Figure 2. Preoperative venography: medial compression of the
popliteal vein in varicose vein recurrence.

Figure 3. Preoperative venography: severe medial compression in a
young athlete.
Surgery was performed under general anesthesia.
– The approach was as follows:
• In three cases, internal approach to the ring of the soleus muscle in the case of low-situated compression (two cases), repeat procedure for four varicose vein recurrences (one case).
• In 8 cases, posterior approach with a transverse incision 1 fingerbreadth from the point of flexion of the knee, and vertical or oblique extension as required during the dissection. Thus, the patient was installed in the prone position with his or her feet extended over the edge of the operating table to allow perioperative maneuvers.
A long vertical aponeurotomy provided the approach to the area. At the end of the procedure, it was converted into an aponeurectomy by resection of a triangular strip to prevent any compression upon closure.
In the case of varicose vein recurrence, an injection of sclerosing foam was administered, using a short 18 G catheter, at the periphery to limit additional phlebectomies and bleeding during the dissection. The sclerosing foam was obtained using Tessari’s whirlpool method, with 1 part Lauromacrogol 1% and 4 parts air collected through a filter. The popliteal vein was located and progressively dissected. Small collateral vessels located on the lateral and posterior aspects were ligated with absorbable 3/0 suture thread. In the case of a neojunction, the latter was sectioned on a level even with the popliteal vein using sutures with 5/0 nonabsorbable single suture thread. The perforating vessels in the popliteal fossa were treated in the same manner. By extending the dissection of the popliteal vein upwards, the anatomy of insertion of the gastrocnemus muscle was identified. In the case of abnormal insertion: three muscle heads, with lateral insertion, disinsertion was performed. Similarly, any muscular component crossing the vein (plantaris muscle) was sectioned. The vein was “cleaned” of all adventitial fibrous material.
After releasing the venous axis, movements of flexionextension of the foot were performed to aid in verifying the absence of compression by a muscular or residual fibrous component.
In the four patients who underwent surgery, a muscle stimulator was used to obtain active contractions, similar to the actual triggering clinical situation.
Drainage with a Redon drain was installed. Aponeurectomy was performed with closure of the skin. The patient was allowed to ambulate on the evening of the day of the procedure and was discharged the next day, wearing an elastic compression stocking for 1 week. The following abnormalities were found:
• a third head of insertion of the gastrocnemius muscle: two cases;
• high and lateral insertion of this muscle: three cases;
• globular hypertrophy of the muscle: six cases;
• hypertrophy of the plantaris or popliteal muscle: four cases (Figure 4);
• perivenous fibrosis: seven cases;
• a fibrous strip crossing the vein: three cases;
• a postsurgical bend: three cases.
ie, a mean of about three abnormalities per patient.
Therefore, it is difficult to refer to a functional syndrome because surgery always revealed one or more anatomical causes of compression.
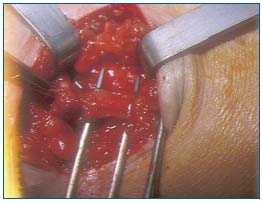
Figure 4. Perioperative view: hypertrophied popliteal muscle prior
to sectioning.
RESULTS
Patients were seen again 1 month after the procedure, and then at repeat visits at 6 months and 1 year. Longterm monitoring was initiated with a hemodynamic evaluation every 2 years, except for patients with a varicose vein recurrence who were seen yearly.
Symptoms improved in nine out of 11 patients. The two patients who remained symptomatic underwent repeat surgery for aponeurotomy of the tibialis muscle in the setting of a compartmental syndrome. Both of these patients were athletes who had resumed training during the weeks following surgery. Heaviness in the calf muscle persisted in two patients, one of whom had sequelae of sural vein thrombosis.
The clinical signs, ie, positional edema, present prior to surgery in all of the patients, showed lasting improvement in eight: two presented with a recurrence on a more moderate level and did not undergo repeat surgery. In the two cases, edema was manifest in the seated position.
Calf circumference was increased by over 2 cm compared with the opposite calf in nine patients. It decreased by 1.5 cm on average in six, less than 1.5 cm in three, and was unchanged in two others.
In the last five patients who underwent surgery, an SF 12 Quality-of-Life questionnaire was filled out before the procedure, and at the first two repeat visits. It demonstrated a significant improvement with a mean of 34 before and 8 after surgery.
The four patients with repeated varicose vein recurrence who underwent surgery did not present any major recurrence during follow-up. Three of them underwent sclerosing therapy of collateral veins at the visits of 1 and 2 years.
The hemodynamic evaluation confirmed the elimination of extrinsic compression in the nine patients who underwent surgery.
The other two underwent repeat venography, which showed the persistence of a positional imprint that was less pronounced than preoperatively.
DISCUSSION
We diagnosed extrinsic compression of the popliteal vein in three different clinical situations:
• in active patients, often athletes, or patients whose occupation promoted hemodynamic decompensation;
• in patients who underwent surgery for an incompetent short saphenous vein;
• in the case of a recurrent sural vein thrombosis.
1/ Popliteal vein entrapment in athletes
By examining asymptomatic subjects, ie, medical students, Nicolaïdes2 demonstrated the existence of postural impairment to emptying of the popliteal vein in 25% of cases.
Anatomical variations in the popliteal fossa are common, and bear witness embryonic development. Some variations consist of the existence of an additional bundle for insertion of the gastrocnemius muscle, which becomes the artery, and the manifestation of ischemic disorders. Other variations are less pathogenic: high, lateral insertion of this muscle, producing conditions favorable to venous compression in the case of an additional factor.
Currently, this factor is represented by athletic activity, especially in young women.
The practice of a sport that results in overdevelopment of the calf muscle, eg, weight lifting (bench press), is often a precipitating factor: we found this in 5 out of 7 subjects who underwent surgery.
In a series of 30 cases reported by Turnipseed,3 27 were confirmed athletes whose mean age was 24 years.
Should these young women be subjected to surgery, which leaves a long scar, and whose cosmetic result cannot be guaranteed (frequent occurence of keloids in this area)?
Raju and Neglen4 reported of 30 patients treated with surgery which can help to provide an answer. Their patients’ mean age was clearly higher (49 years), 30% of them presented with advanced venous insufficiency with varicose ulcers. This internationally renowned team received patients considered as difficult cases, and thus there was a selection bias.
However, it is possible to consider that among subjects diagnosed at a young age, a significant percentage run the risk of progressing to chronic venous insufficiency if the obstacle to venous drainage is not removed. In addition, these subjects wish to resume their athletic activity: 24 of the 27 athletes operated on by Turnipseed resumed training under good conditions.
The surgical approach allows a less damaging procedure: Raju uses an internal approach, Turnipseed a short posterior medial approach focused on the insertion of the gastrocnemius. However, these limited approaches do not allow extended dissection of the popliteal vein, and thus run the risk of inadequate release with subsequent recurrence.
It may be useful to study a laparoscopic approach to the area in an effort to diminish the cost of a resultant scar.
Can the occurrence of this syndrome be prevented?
In an anatomically predisposed area, all subjects do not present with symptoms.
Nicolaïdes did not follow the long-term course and outcome of his medical students who had a hemodynamic obstacle: how many of them became symptomatic?
In the setting of sports medicine, it may be possible to consider having young women who engage in a “highrisk” sport answer a questionnaire aimed at screening to detect positional compression. In the case of replies suggesting this, a hemodynamic evaluation with duplex scanning would be ordered. The training program should then be adapted to take into account hemodynamic fragility, in particular avoiding contractions of the calf muscle in response to heavy loads, and by working more on elongation.
Another possibility would be perform an isolated aponeurectomy, which requires a small incision, but which could be sufficient to decrease the pressure exerted on the vein. The relationship found by some authors between popliteal vein entrapment and a compartmental syndrome encourages us to attempt this relatively noninvasive solution.
2/ Popliteal vein entrapment and varicose vein surgery
Four of our operated patients had undergone surgery for treatment of varices: one simultaneous resection of the long and short saphenous veins, three stripping of the short saphenous vein. All of them had presented with rapid-onset recurrence of varicose veins, 6 to 18 months after the first procedure. All of them had undergone repeat surgery at least once, and two had undergone three procedures!
The relationships between extrinsic compression of the popliteal vein and varices lie on several levels:
• Compression revealed by stripping
The saphenous veins are the main pathway of collateral circulation of obliteration of the popliteal vein in the case of a popliteal thrombosis. Acceleration of saphenous blood flow seen with Doppler scanning is a constant sign of this. Depending on the level of compression, the deep blood flow will be shunted either by the short or the long saphenous vein, as Gillot demonstrated in his venographic studies.5
Elimination of this collateral circulation can decompensate a fragile hemodynamic situation. The obstructive syndrome in the deep venous network then induces the recurrence of varices, which are accessory drainage veins. This process is explained, for example, by the secondary occurrence of reflux by the popliteal perforator vein following surgery of the short saphenous vein.
As long as the deep obstacle is not removed, varices recur, as was the case in our four patients.
• Compression induced by stripping
In a “borderline” anatomical situation, stripping can result in compression if the aponeurotomy of the saphenopopliteal junction is horizontal and if it is sutured at the end of the surgical procedure. This suture narrows the popliteal fossa and promotes postural compression.
Raju also believes that the stumps of a crossectomy can induce the formation of a fibrous tract that can produce a bend in the popliteal vein in some positions.
How to avoid these complication
In the preoperative assessment, it is important to detect popliteal vein entrapment, especially prior to surgery on the short saphenous vein.
Here too, as in athletes, the interview can provide pointers. A hemodynamic evaluation will be ordered. If positive, there should be no hesitation in ordering dynamic venography before performing an intervention. Prevention of an iatrogenic syndrome is based on making a vertical unsutured aponeurotomy at the end of the procedure. It is also necessary to ligate and section the collateral vessels, which can produce a bend in the popliteal vein. The operator should remember to perform dynamic maneuvers during the procedure.
3/ Recurrent sural vein thrombosis
Two of our patients presented with a sural vein thrombosis, which recurred during the months following the end of anticoagulant therapy. Laboratory tests did not reveal any coagulation abnormalities such as thrombophilia. Wakefield6 has described this possible etiology and the possible resultant sequelae.
This problem can be suspected based on clinical findings when calf edema persists in spite of deep repermeation, and does not improve a few months after an acute episode. If the diagnosis is not established, these patients will be seen at the stage of chronic venous insufficiency, which was the case of Raju’s surgically treated patients. Our two patients with this disorder who underwent surgery have not had a recurrence 2 and 4 years after the procedure.

REFERENCES
2. Leon M, Labropoulos N, Nicolaïdes A. Popliteal vein entrapment in the normal population. Eur J Vasc Endovasc Surg. 1992;6:623-627.
3. Turnipseed W. Popliteal entrapment syndrome. J Vasc Surg. 2000;35:910-915.
4. Raju S, Neglen P. Popliteal vein entrapment: a benign venographic feature or a pathologic entity? J Vasc Surg. 2000;31:631-641.
5. Gillot C. Les obstacles posturaux de la veine poplitée. Phlébologie. 1992;45:265- 286.
6. Gerkin TM, Beebe HG, Wakefield TW. Popliteal vein entrapment presenting as deep venous thrombosis and chronic venous insufficiency. J Vasc Surg. 1993;18:760-766.
