Overview of the advances in thermal ablation techniques. Where do we stand?
Dimitrios Kontothanassis,
MD, Prof, MS
Department of Phlebology, Istituto
Flebologico Italiano, Padova, Italy
General and Vascular Surgeon,
CEO Istituto Flebologico Italiano,
Padova, Italy
ABSTRACT
Varicose veins are a very common condition and have been the subject of a recent proliferation of treatment modalities. The last 2 decades have seen extraordinary expansion in superficial venous surgery. Traditional surgical procedures (crossectomy and stripping) are now being replaced to a greater or lesser extent by new, less invasive endovenous methods, but the advent of the endovenous treatment era has led to a confusing array of different modalities of treatment. This paper provides an overview of the advances in thermal ablation techniques. All modalities offer excellent results in the right situation, and each has its own treatment profile. Endovenous thermal ablation techniques have matured and have a reassuring and reliable outcome. Our aim is to provide an up-to-date review of all available endovenous thermal techniques (laser, radiofrequency, steam), describing the indications, the procedure, mechanism of action, and the outcomes. In experienced hands, all endovenous techniques are safe and effective, with long-term results comparable to conventional surgical procedures.
Introduction
Endovenous thermal techniques, namely, radiofrequency (RF) ablation, endovenous laser ablation (EVLA), and steam ablation, were introduced around the 21st century and have revolutionized the way varicose veins are treated.1 These minimally invasive techniques are associated with an earlier return to normal activity and less pain, and they enable procedures to be carried out as day cases. However, they are also known to cause a number of side effects and involve infiltration of tumescent fluid, which can cause discomfort.2 On systematic review, the clinical practice guidelines from the Society for Vascular Surgery (SVS)/American Venous Forum (AVF) in 2011 and from the SVS/AVF/American Vein and Lymphatic Society (AVLS) in 2023 highly recommend such techniques (Grade 1b) for the treatment of saphenous incompetence in symptomatic patients over high ligation and stripping (quality of evidence B; Table I).3
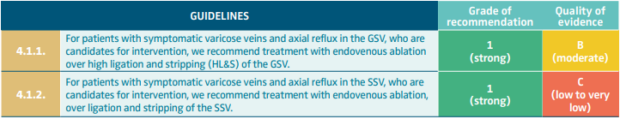
Table I. Endovenous ablation versus high ligation and stripping. From the 2023 SVS/AVF/AVLS Clinical Practice Guidelines for the management of varicose veins of the lower extremities (Part II).
Abbreviations: AVF, American Venous Forum; AVLS, American Vein and Lymphatic Society; GSV, great saphenous vein; SSV, small saphenous vein; SVS, Society for Vascular Surgery.
After reference 3: Gloviczki et al. J Vasc Surg Venous Lymphat Disord. 2024;12(1):101670. © 2023 The Author(s). Published by Elsevier Inc. on behalf of the Society for Vascular Surgery.
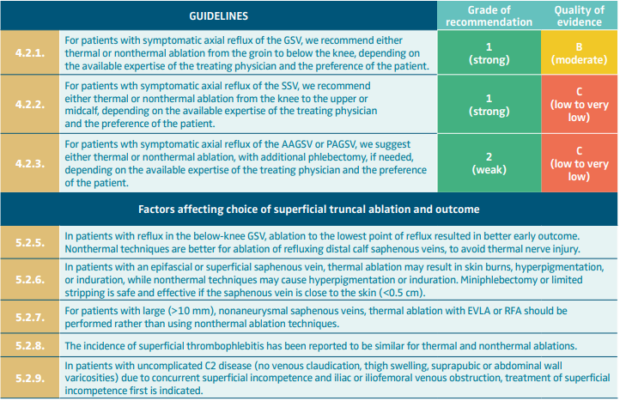
Table II. Top panel) Thermal versus nonthermal ablation of superficial truncal veins. Bottom panel) Factors affecting choice of superficial truncal ablation and outcome. From the 2023 SVS/AVF/AVLS Clinical Practice Guidelines for the management of varicose veins of the lower extremities (Part II).
Abbreviations: AAGSV, anterior accessory great saphenous vein; AVF, American Venous Forum; AVLS, American Vein and Lymphatic Society; EVLA, endovenous laser ablation; GSV, great saphenous vein; PAGSV, posterior accessory great saphenous vein; RFA, radiofrequency ablation; SSV, small saphenous vein; SVS, Society for Vascular Surgery.
After reference 3: Gloviczki et al. J Vasc Surg Venous Lymphat Disord. 2024;12(1):101670. © 2023 The Author(s). Published by Elsevier Inc. on behalf of the Society for Vascular Surgery.
Although RF ablation was the pioneer endovenous technique introduced in 1998, laser ablation introduced immediately afterward in 1999 spread globally and faster with very promising results. The 810-nm and 980-nm diode laser using bare fibers dominated the global scientific scene for at least 5 years up to 2005 because results were much better than with the first generation of RF generators. The second generation of RF generators (ClosureFast) achieved better results in terms of closure rates after saphenous ablation, reduction in postoperative pain, and less bruising than with the 810-nm and 980-nm diode laser. Results were equalized again after the introduction of new wavelengths for laser devices (1470 nm and 1940 nm) and development of new high-quality fibers (radial optical fibers, single or double ring, normal or slim). New promising results are being observed with the next-generation RF generator (Venclose), which is a multi-voltage energy delivery system with touchscreen control that automatically sets the nonadjustable treatment parameters for the Venclose System Catheters. The author believes that this technique, with proper studies in future trials, should seek to standardize the modality of treatment and the clinical terminology, and that it will provide more evidence on outcomes of treatments on long-term follow-up. Steam was introduced in 2011 but never spread globally; even today, it accounts for only a small part of thermal and tumescent procedures.
However, the 2023 SVS/AVF/AVLS clinical practice guidelines recommend either thermal or nonthermal ablation from the groin to below the knee, depending on the available expertise of the treating physician and the preference of the patient. For patients with large (>10 mm), nonaneurysmal saphenous veins, thermal ablation with EVLA or RFA should be performed rather than using nonthermal ablation techniques. (Table II-5.2.7).3
How it works
All endothermal techniques can be offered as outpatient procedures that can be done under local anesthesia. Proper evaluation of a patient’s condition has to be done so that in high-risk patients a further evaluation of risk factors prior to operation can be offered. For patients that present emotional problems, a combination of oral or endovenous mild sedation can be given in addition to local anesthesia. All techniques require ultrasound assistance to perform vascular access, navigate inside the vein, target and identify the correct point of entry into the vein, and landmark the point for starting a correct ablation. All techniques can be done by using a 16–18-gauge needle and inserting a guide wire or using a micropuncture kit. Usually, the sheath used for vascular access is 6F; no sheath is required for the steam procedure.
Tumescent anesthesia is mandatory for thermal techniques, and large amounts of tumescent liquid have to be delivered around the vein in order to dissect it from the surrounding tissues and cause extreme spasm of the vein wall around the catheter (Figure 1).
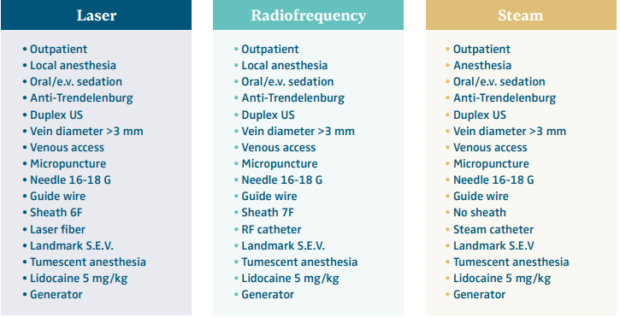
Figure 1. Set up of endothermal procedures: left) laser; center) radiofrequency; and right) steam.
Abbreviations: e.v., endovenous sedation; RF, radiofrequency; US, ultrasound. Courtesy of Prof D. Kontothanassis.
Contraindications to endothermal ablation techniques
For all endothermal techniques, it is very important to assess all the contraindications to transcatheter ablation (Figure 2) and to use the following criteria to make your treatment selection:
• Presence of anatomical variability of saphenous veins (duplication, aplasia, hypoplasia, extra fascial saphenous veins).
• Distance between the vein and the skin (is it >3 mm?).
• Presence of dilatation and tortuosity of the saphenous vein axis. (Do not treat veins with a diameter >25 mm unless you are very skilled in EVLA).
• Integrity of the deep venous system, assessed by excluding the presence of deep venous thrombosis (DVT) or venous narrowing after DVT.
• Patency of the great saphenous vein (GSV) and the small saphenous vein (SSV) before the operation.
Complications of endothermal techniques
The most common intraoperative complications of thermal techniques are the inability to cannulate the target vein or to advance the endovenous ablation catheter, an allergic reaction to tumescent anesthesia, a vasovagal response, hypotension, and bleeding. Postoperative complications are thrombophlebitis, endovenous heat-induced thrombosis (EHIT), pulmonary embolism, skin burn, discoloration, paresthesia, chronic pain, numbness, infection, hematoma, bruising, and persistent patency of the ablated vein. Table III shows complications of endovenous ablation in randomized controlled trials.4
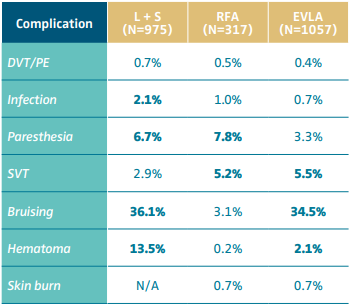
Table III. Complications of endovenous thermal techniques in randomized controlled trials.
Abbreviations: DVT: deep venous thrombosis; EVLA, endovenous laser ablation; L+S, conventional ligation plus stripping; N, number of treated limbs; PE, pulmonary embolism; RFA, radiofrequency ablation; SVT, superficial venous thrombosis or thrombophlebitis.
Based on reference 4: Dermody M, O’Donnell TF, Balk EM. J Vasc Surg Venous Lymphat Disord. 2013;1:427-436.e1.
Treatment of below-knee veins
Below-knee veins are often problematic to treat with thermal techniques because of the high risk for injury of the saphenous vein (SV). During harvest of the SV, the most important relationship to take into account is the saphenous nerve (SN) in order to avoid pain and paresthesia after surgery. The most vulnerable area is the inferior third of the leg because of vein and nervous adhesion. Use of large amounts of tumescent anesthesia aims to completely separate the vein from all the other tissues and prevent nerve damage (Figure 3). When the risk of nerve damage during ablation is high, one should ask the patient to report any pain or electric stimulation and stop immediately if the answer is positive. In case of risk of nerve injury, you can reduce the amount of the delivered energy or pull back the laser fiber or the RF catheter 1 to 2 cm. Thanks to its longer wavelength, the 1940-nm diode laser is very promising for treating below-knee veins; this innovative endovenous laser requires significantly less energy. However, these promising results are for a 3-year follow-up period, whereas long-term results, greater than 10 years, are needed.
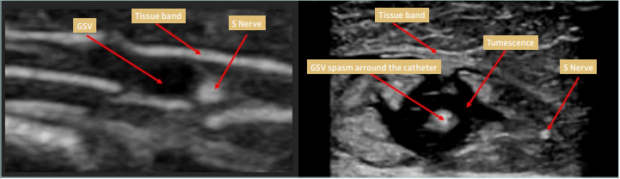
Figure 3. High volume tumescent anesthesia to separate the saphenous nerve from the saphenous vein.
Abbreviation: GSV, great saphenous vein. Courtesy of Prof D. Kontothanassis.
How much energy dispense is needed
to ablate the target vein?
to ablate the target vein?
The amount of energy depends on the individual vein, and this is the biggest difference between standardized and nonstandardized techniques. The risk associated with increasing the delivered energy rate for laser (J/cm) using different wavelengths is perforation of the vein wall. Usually, the higher the laser wavelength the less energy required for treating target veins, but it is very difficult to standardize. RF catheters for vein ablation (standardized techniques) deliver thermal energy constantly and uniformly via a dedicated microprocessor-controlled generator.
With the new devices that generate heat at 120 °C, boiling, vaporization, and carbonization of the tissues are avoided. The temperature of the electrodes (7- or 10-cm length) has increased from 120 °C (second-generation RF; Medtronic) up to 130 °C (next-generation electrode; Venclose, BD). The heating element is energized by the Venclose RF Generator, which is a multi-voltage energy delivery system with touchscreen control that automatically sets the nonadjustable treatment parameters for the Venclose System Catheters. A button on the catheter begins an automated treatment cycle 20 seconds long at a set temperature of 130 °C (Venclose RF Ablation Catheter). The treatment stops automatically when complete.
The procedure of steam ablation is very similar to EVLA, and it is a nonstandardized thermal technique. Though a step-by-step procedure is lacking in the literature, after activation, the catheter releases small “puffs” of steam, and the catheter is pulled back in a stepwise manner. A physicist calculated that approximately 2258 J is released when 1 g of steam condenses.5
Histological findings and results
During endovenous RF ablation, the thermal energy delivered to the venous segment to be treated causes direct injury with acute and posttreatment effects. Acute endovenous RF ablation effects of thermal injury are endothelial denudation, thickening of the vein wall, contraction of the vein wall collagen fibrils, and necrosis of the smooth muscle and vein wall components. Posttreatment effects of thermal injury are extensive growth of fibroblasts, new collagen synthesis, further thickening of the vein wall, and a further fibrotic sealing of extensively narrowed vessels (Figure 4).
Microscopic examination of veins immediately after steam ablation showed disappearance of the endothelial layer. Microscopic examination of treated veins that were removed 20 days after steam ablation showed endothelial destruction, fibrotic thrombosis with inflammatory reaction of the media, major alterations of elastic and collagen fibers in the media, and lesions in the adventitia with liponecrosis and lipogranuloma (Figure 5).
Microscopic examination of veins immediately after laser ablation showed eosinophilia, congestion, thrombosis, as well as necrosis of the endothelium. With regard to the periadventitial tissues, there was evidence of fragmentation of connective fibers and adipose areolas, as well as brownish deposits of burnt material (Figure 6).
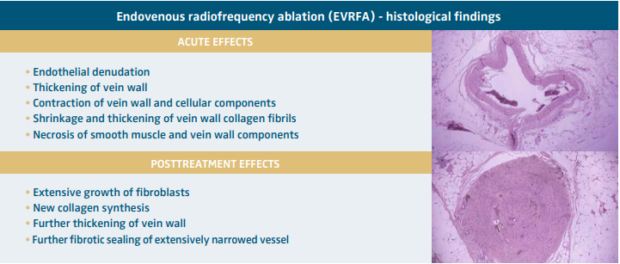
Figure 4. Histological findings after radiofrequency ablation.
Abbreviation: EVRFA, endovenous radiofrequency ablation. Images courtesy of R. Weiss and M. Goldman. Courtesy of Prof D. Kontothanassis.
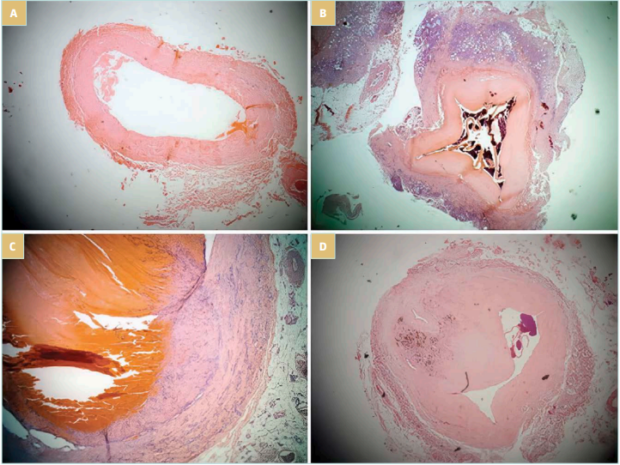
Figure 5. Microscopic examination after steam ablation: A) immediately after steam ablation; B,C) after 20 days; and D) after 3 months.
After reference 5: van den Bos et al. J Vasc Surg. 2011;53(1):181-186. © 2011 Society for Vascular Surgery. Published by Mosby, Inc. All rights reserved.
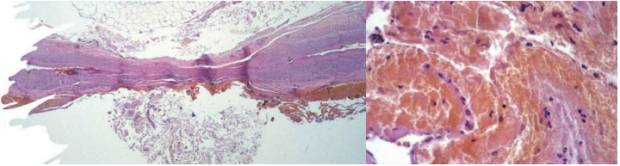
Figure 6. Microscopic examination (histological findings) after endovenous laser ablation.
Courtesy of Prof D. Kontothanassis
Conclusion
Early treatment of symptomatic chronic venous disease (CVD) improves quality of life, signs, and symptoms; it slows down progression, but cannot prevent recurrence of varicose veins.1,2,6 RF ablation and laser ablation are both equal and highly recommended techniques for treatment of CVD.4 The recanalization rate during follow-up is the same for both techniques, but the occlusion rate does not reflect clinical success. There is no difference in postoperative pain and bruising. The use of laser needs a longer learning curve than RF. The RF Venclose system is designed for more efficiency and can be considered the next-generation thermal system, but long-term follow-up evaluation is mandatory. Venclose RF can be 30% faster than other thermal techniques because of the 10-cm heating electrode, which can reduce the overall procedure time and cost of operation. Both RF ablation and EVLA should be offered in combination with foam and glue when necessary to achieve better outcomes when dealing with complex vein anatomy.2
International guidelines, multiple reviews, and long-term follow-up studies available in the literature clearly support thermal techniques rather than nonthermal techniques. When comparing RF and laser with foam we have to keep in mind that we are comparing standardized techniques with nonstandardized techniques, and that clinical practice guidelines support thermal techniques when dealing with larger-diameter veins (> 10 mm).3
Reduced time of operation and number of treatment sessions is clearly achievable with thermal techniques when treating full-length GSV, GSV plus anterior saphenous vein, bilateral GSV or SSV; there is no risk in using thermal techniques in patients with patent foramen ovale and for below-knee ablation.

CORRESPONDING AUTHOR
Dr Dimitrios Kontothanassis MD
Via N. Tommasseo 50
– 35131 Padova, Italy
EMAIL: direzione@istitutoflebologico.it
References
1. Davies AH. The seriousness of chronic venous disease: a review of real-world evidence. Adv Ther. 2019;36(Suppl 1):5-12.
2. Kontothanassis D. Endovenous Ablation Techniques. Mastering Endovascular Techniques, Tips and Tricks in Endovascular Surgery. Springer; 2024:721-730.
3. Gloviczki P, Lawrence PF, Wasan SM, et al. The 2023 Society for Vascular Surgery, American Venous Forum, and American Vein and Lymphatic Society clinical practice guidelines for the management of varicose veins of the lower extremities. Part II: Endorsed by the Society of Interventional Radiology and the Society for Vascular Medicine. J Vasc Surg Venous Lymphat Disord. 2024;12(1):101670.
4. Dermody M, O’Donnell TF, Balk EM. Complications of endovenous ablation in randomized controlled trials. J Vasc Surg Venous Lymphat Disord. 2013;1:427-436. e1.
5. van den Bos RR, Milleret R, Neumann M, Nijstenet T. Proof-of-principle study of steam ablation as novel thermal therapy for saphenous varicose veins. J Vasc Surg. 2011;53(1):181-186.
6. Raffetto JD, Mannello F. Pathophysiology of chronic venous disease. Int Angiol. 2014;33(3):212-221.

