Iliocaval reconstruction in a patient with chronic deep vein thrombosis caused by retroperitoneal fibrosis
Affiliations: 1. Department of Cardiovascular Surgery, Faculty of Medicine, Acibadem University, Istanbul, Turkey. 2.
Department of Cardiovascular Surgery, Acibadem University Atakent Hospital, Istanbul, Turkey. 3. Department of Radiology, Acibadem University Atakent Hospital, Istanbul, Turkey. 4. Department of Cardiovascular Surgery, Acibadem Altunizade Hospital, Istanbul, Turkey
Retroperitoneal fibrosis (RPF) is a rare condition characterized by excessive fibrotic tissue growth in the retroperitoneum, often leading to vascular and ureteral compression. Chronic deep vein thrombosis (DVT) resulting from RPF can cause significant venous outflow obstruction and debilitating symptoms. Endovascular venous stenting has emerged as a minimally invasive and effective treatment option for restoring venous patency and alleviating symptoms in these complex cases.
A 26-year-old female patient was admitted to our clinic with complaints of bilateral lower-extremity swelling and visible abdominal wall vessels. Twenty months earlier, she experienced acute-onset abdominal pain. Imaging revealed a retroperitoneal mass around the inferior vena cava (IVC) and abdominal aorta at the renal level. A biopsy confirmed RPF. Two months after the diagnosis, she developed acute bilateral lower-extremity swelling and pain. Ultrasound and computed tomography venography (CTV) showed acute DVT extending from the level of the fibrosis to the iliac veins. She was treated with low-molecular-weight heparin and oral anticoagulants, but her symptoms did not improve. She also experienced venous claudication after walking 100 meters. Magnetic resonance venography revealed chronic thrombosis of the infrarenal IVC, right common and external iliac veins, right common femoral vein, and left common iliac vein (Figure 1).
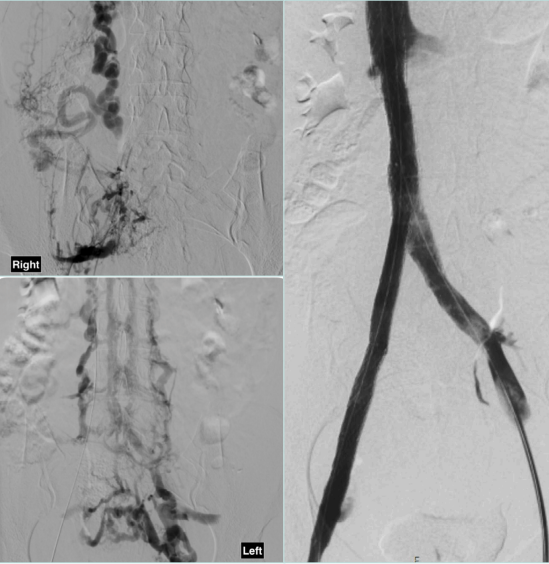
We planned to perform endovascular iliocaval reconstruction. Using bilateral femoral vein access, we conducted venography, which revealed numerous collateral veins filling the proximal IVC and azygos veins (Figure 2). We successfully crossed the lesions from both sides. After aggressive predilation, an 18 mm x 120 mm Abre venous stent was placed in the IVC. Subsequently, a 14 mm x 150 mm and a 12 mm x 120 mm Abre venous stent were implanted from the right common iliac vein to the femoral vein, and a 14 mm x 120 mm Abre venous stent was implanted in the left common iliac vein using the kissing technique. After postdilation, control venography showed that the collaterals had disappeared and the flow was very satisfactory (Figure 2). The venous stents remained patent on the first-year CTV scan.
Iliocaval reconstruction is a viable and effective option for the management of chronic DVT caused by RPF. This approach not only addresses the underlying venous obstruction but also alleviates symptoms, improves venous outflow, and enhances the quality of life for affected patients. Proper patient selection, meticulous preoperative imaging, and individualized surgical planning are essential to optimize outcomes.
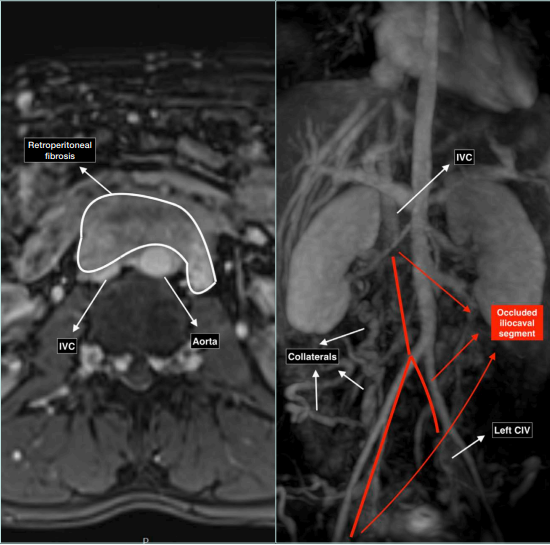
Figure 1. Preoperative magnetic resonance venography showing compression of the vena cava by retroperitoneal fibrosis and iliocaval venous occlusion. CIV, common iliac vein; IVC, inferior vena cava.