Anatomy of foot and ankle perforator veins
Miguel LO VUOLO2
Claude GILLOT1
Descartes University, Paris Cité Sorbonne
2 Diagnóstico por Imágenes Junín,
Santa Fe, Argentina
Abstract
Background: The foot venous pump is located in the plantar veins, where both its anatomy and connections with the saphenous roots and the foot perforator veins are not well known, and therefore, they are under investigated in daily practice. The aim of this paper is to describe the unique anatomy and the functional role of the foot perforator veins and emphasize their key role during the activation of the foot venous pump. Ankle perforator veins also play a crucial role in the venous blood return, giving rise to the anterior tibial and fibular veins.
Materials and methods: A total of 400 cadaveric feet from the “don des corps” of the Descartes University (Paris, France) were injected with green Neoprene latex, which was followed by an anatomical dissection and a colored segmentation of the venous system. Duplex color sonography and CT venography with 3D modeling were used to investigate the foot perforator veins and their connections with the foot venous pump and the saphenous systems in patients with venous disease.
Results: Some foot perforating veins are characterized by flow that is oriented from deep to superficial veins, due to the presence of one-way valves, a unique feature in the venous system of the lower limbs. From a hemodynamic point of view, the foot veins should not be classified into deep and superficial systems, but into medial and lateral functional units. The medial unit is comprised of the medial plantar veins, the medial marginal vein, and the medial foot perforator veins. The lateral unit is comprised of the lateral plantar veins, the lateral perforator veins, and perforator veins of the calcaneus. Ankle perforator veins are mainly the dorsal perforator veins that are connected to the initial segment of anterior tibial and fibular veins and the lateral perforator veins along the distal fibula.
Conclusion: Despite the small volume of blood ejected at each step, the foot venous pump plays a key role in the venous blood return of the lower limbs. The foot perforator veins are the main outlet of the foot venous pump into the superficial venous system, working from deep to superficial; therefore, they are responsible for the systolic ascending flow in both the great and small saphenous systems during foot venous pump activation.
Anatomical technique and protocol
The injection technique has been described previously in our anatomical study of the foot venous pump.1,2 This study used 400 feet from 200 nonselected, nonembalmed cadaveric subjects from the department of the “don des corps” of the Descartes University (Paris, France), with an average age of 84. After exposing the medial marginal vein, a No. 19 butterfly venous catheter was inserted and directed toward the toes (countercurrent to the physiological blood flow). The common femoral vein was approached, and a tube was inserted to perform lavage-irrigation with soapy water, which was repeated several times, followed by a massage of the muscles to obtain a clear liquid. After ligating the common femoral vein, it takes about 30 minutes to fill the entire venous network by injecting 120-150 mL of green neoprene latex in each limb. Dissection was performed on the following day, and color segmentation was done by painting veins with different dyes to simplify their identification.
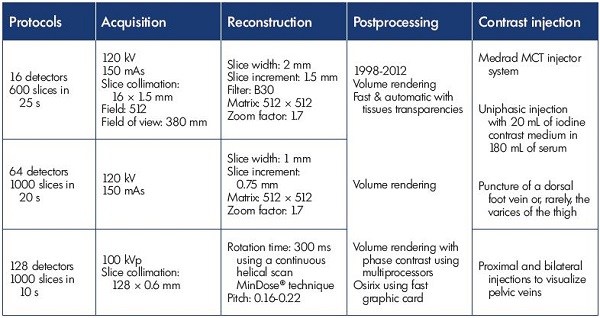
Color Doppler ultrasound was used to assess the anatomy of the foot perforator veins, their connections with the foot venous pump, and their hemodynamics. Multislice CT venography (also known as phlebo CT) was used to obtain the 3D modeling of the foot’s venous system, which strongly correlated with the dissection findings. Multislice CT venography was specifically indicated for patients with a complex venous disease or recurrent varices after surgery (REVAS). The multislice CT venography acquisition and reconstruction protocol and results (Table I) have been described previously.3-5 This technique provides an accurate depiction of the foot veins, with an interactive 3D assessment, including virtual dissection. These new imaging tools also provide access to virtual reality techniques,6,7 which is mainly the virtual dissection of the limb, and it is useful for making decisions in complex cases, for educational purposes, and to improve our knowledge of the venous anatomy.
Foot pump anatomy
The venous blood reservoir of the foot, also called the foot venous pump, is located deeply in the plantar veins, between two plantar muscles, the quadratus plantaris, and the Hallux flexor longus (Figure 1).1,2 The medial (or internal) plantar pedicle is short (5 cm), rectilinear, and it is comprised of 2 to 3 veins that are often plexiform with several anastomoses. The lateral (or external) plantar pedicle is longer (12 cm), curved, and larger. It is located between the two muscle layers of the sole; therefore, it is compressed during the systolic phase of the foot venous pump. The lateral plantar pedicle is comprised of 2 to 3 veins (2 to 4 mm in diameter), which are connected to each other by several anastomoses (Figure 2). These two plexiform pedicles join posteriorly to form the calcaneus confluent of the plantar veins, where the blood is ejected upward into the posterior tibial veins, which are the main exit pain of the foot venous pump.1,2
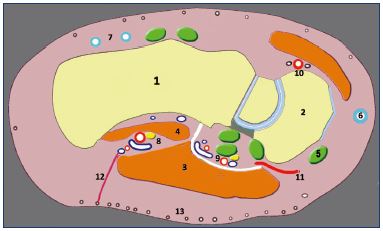
Figure 1. Paramedial longitudinal section of the foot.
This section shows the intermuscular topography of the lateral
plantar veins (8) located in the slit that separates the fleshy body
of the quadratus plantaris (4) from that of the abductor hallucis
(3). The medial plantar veins (9) have fibrous and tendinous
relations.
Abbreviations: 1, calcaneus bone; 2, navicular bone; 3, abductor
hallucis; 4, quadratus plantaris; 5, tendon of the posterior tibial
muscle; 6, medial marginal vein; 7, lateral marginal plexus; 8,
lateral plantar veins; 9, medial plantar veins; 10, pedal artery;
11, navicular perforator vein; 12, perforator in fatty tissue;
13, subcutaneous venous plexus of the sole.
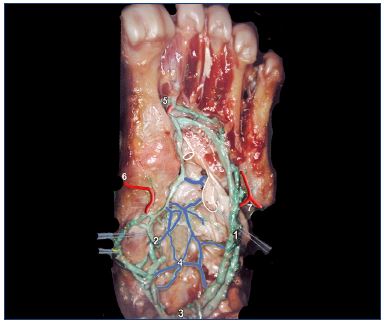
Figure 2. Anatomical dissection of foot veins (inferior view).
Latex injection and colored segmentation.
Abbreviations: 1, lateral plantar veins (double); 2, medial
plantar veins; 3, calcaneal crossroad of the plantar veins; 4,
plexus-shaped network of the sole; 5, perforator of the first
intermetatarsal space; 6, navicular perforator; 7, perforator of
the fifth metatarsal bone.
Figure 3 shows the complete anatomy which explains foot venous pump function. The pump (shown in green), which is comprised of plantar veins, has three parts (listed from front to back)–a suction pole (A), a reservoir (R) in the plantar veins, and an ejection pole (C) at the calcaneal confluent. Anteriorly, at the aspirational pole, blood enters the pump during relaxation of the plantar muscles during the foot’s plantar flexion. The ejection pole is represented by the calcaneal confluent or calcaneal crossroad (C). During foot venous pump systole, blood is ejected directly toward the posterior tibial veins and the great and small saphenous veins through the foot perforator veins.
For a more detailed description, please see our previous paper: Phlebolymphology. 2010;17:151-158.2
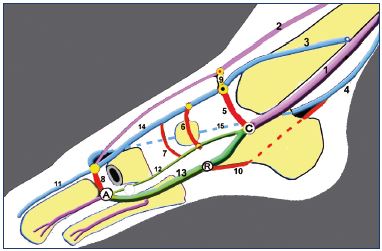
Figure 3. Hypothesis about venous pump function.
The three parts of the foot venous pump include a suction pole
(A), a reservoir (R) in the plantar veins, and an ejection pole (C)
at the calcaneal confluent.
Abbreviations: 1, posterior tibial vein; 2, anterior tibial vein; 3,
great saphenous vein; 4, small saphenous vein; 5, submalleolar
perforator; 6, navicular perforator vein; 7, cuneal perforator vein,
8, perforator vein of the first intermetatarsal space; 9, dorsal
perforator vein; 10, calcaneal perforator vein; 11, dorsal vein of
the hallux; 12, medial plantar vein; 13, lateral plantar vein; 14,
medial marginal vein; 15, lateral marginal network (dotted line).
Anatomy of the foot perforator veins
Foot perforator veins provide direct connections between the plantar veins and the roots for both saphenous systems. These foot perforator veins are split into two well separated functional units (medial and lateral), connected to each plantar vein. The medial foot perforator veins are connected to the medial plantar veins and the roots for the great saphenous vein. Lateral and posterior or calcaneal foot perforator veins are connected to the larger lateral plantar veins and the roots for the small saphenous vein. The anterior foot perforator veins also connect the dorsal foot network to the origin of the fibular and anterior tibial veins at the ankle.
Medial foot perforator veins
The perforator veins of the first intermetatarsal space, generally with a large diameter (4 mm), is at the anterior aspect of the dorsal foot. It originates from the medial marginal vein, which is the main root for the great saphenous vein below the medial malleoli (Figures 4 and 6). The three medial perforator veins of the foot include: (i) the inframalleolar perforator, which is the second root for great saphenous vein; (ii) the navicular (or scaphoid) perforator, which is close to the navicular bone; and (iii) the cuneal perforator, which is located next to the first cuneal bone. The dorsal medial perforator communicates anteriorly with the anterior tibial veins, and it often forms laterally to the third root for the great saphenous vein (Figures 3 and 4).
Lateral foot perforator veins are cuboid or tendinous perforators
Lateral foot perforator veins are comprised of two veins crossing the lateral fibular tendons that are also called intertendinous and subtendinous perforator veins (Figures 5 and 8). These two perforator veins frequently join into a common trunk, which connects to the lateral marginal network, giving rise to the main root for the small saphenous vein.
Calcaneal foot perforator vein is a posterior foot vein
The calcaneal foot perforator vein originates from the calcaneal plexus and usually feeds the Achilleal tributary vein, which runs upward and medially to the Achilles’ tendon, and it commonly joins the small saphenous vein at the lower third of the calf (Figures 6, 7, and 10). To the best of our knowledge, the Achillian tributary has not been previously described. It is important because it establishes a direct connection between the lateral plantar veins and the small saphenous vein.
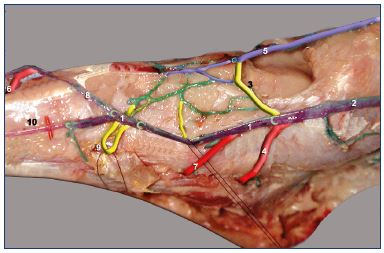
Figure 4. Anatomical dissection of the foot perforating veins
(medial view).
Latex injection and colored segmentation (1, 3, and 4 are the
three roots for the great saphenous vein).
Abbreviations: 1, medial marginal vein; 2, great saphenous
vein; 3, dorsal perforator vein that is communicating with the
anterior tibial vein; 4, submalleolar foot perforator vein; 5,
anterior tibial vein; 6, perforator vein of the first intermetatarsal
space; 7, navicular perforator vein; 8, dorsal arcade of the foot;
9, dorsal perforator vein; 10, dorsal vein of the Hallux.
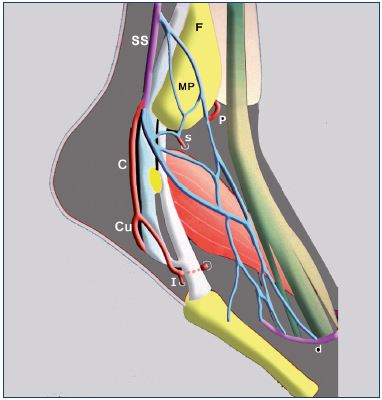
Figure 5. An illustration showing the roots for the small
saphenous vein.
The lateral marginal vein, absent in the majority of cases, is
often replaced by a lateral marginal plexus.
Abbreviations: C, common trunk of the lateral perforator vein;
Cu, cuneal perforator vein; d, dorsal foot arcade; F, fibula;
I, intertendinous perforator vein; MP, malleolar plexus; P, dorsal
perforator vein for the anterior tibial veins; s, dorsal perforator
vein for the fibular veins; SS, small saphenous vein.
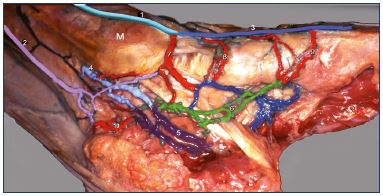
Figure 6. Anatomical dissection of the foot perforating veins
(medial view).
Latex injection and colored segmentation.
Abbreviations: 1, great saphenous vein at the medial malleolus;
2, Achillean tributary of the small saphenous vein; 3, medial
marginal vein; 4, posterior tibial veins; 5, lateral plantar
veins; 6, medial plantar veins; 7, submalleolar perforator
vein; 8, navicular perforator vein; 9, cuneal perforator vein;
10, calcaneal perforator.
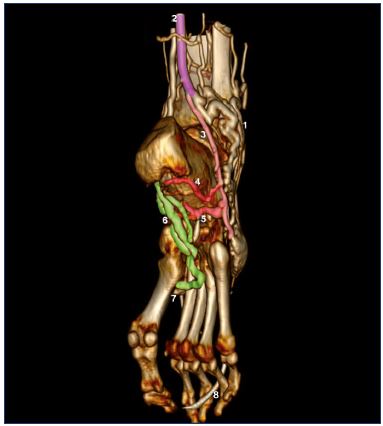
Figure 7. Three-dimensional reconstruction of the foot by CT
venography.
Inferior and lateral view of a right foot.
Abbreviations: 1, varicose network of the lateral marginal
plexus; 2, small saphenous vein; 3, common trunk of the
lateral perforator veins; 4, calcaneal perforator vein; 5, cuneal
perforator vein; 6, lateral plantar veins; 7, perforator vein of
the first intermetatarsal space; 8, venous catheter for contrast
injection.
Anterior perforator veins of the foot and ankle
There are commonly three anterior perforating veins. One is connected to the medial marginal vein, and it is the dorsolateral component of the three great saphenous vein roots. The two other perforating veins come from the venous network of the dorsal foot. They constitute a separate entity, which is not connected directly to the plantar veins, and gives rise to the fibular and anterior tibial veins (Figures 8 and 11).

Figure 8. Anatomical dissection of foot perforating veins (lateral
view).
Latex injection and colored segmentation.
Abbreviations: 1, small saphenous vein; 2, dorsal plexus; 3,
intertendinous perforator vein; 4, cuneal perforator vein; 5,
dorsal perforator veins; 6, anterior tibial veins; 7, fibular veins; c,
common trunk of the lateral perforator veins.
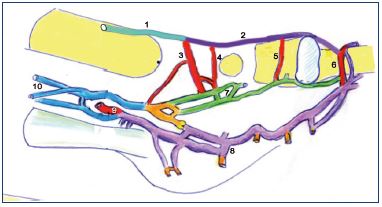
Figure 9. An illustration of foot perforator veins.
The medial functional unit is composed of the medial marginal
vein (2), which continues as the great saphenous vein (1), and
the submalleolar (3), scaphoid (4) and cuneal (5) perforating
veins. The previously mentioned perforator veins (3, 4, and 5),
together with the first intermetatarsal space perforator vein
(6), are connected to the medial plantar veins (7). The lateral
functional unit is composed of the lateral plantar veins (8) and
the calcaneal perforator vein (9). In the rear the plantar veins
join the calcaneal which gives rise to the two confluent (yellow),
originating both plexiform posterior tibial veins (10).
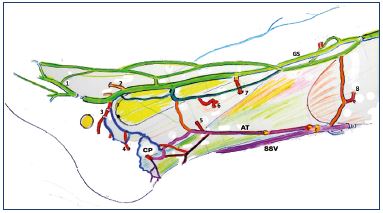
Figure 10. Anatomical dissection, medial view of the Achillean
tributary of the small saphenous vein. Right lower leg.
Abbreviations: 1, medial marginal vein; 2, dorsal perforator vein
to the anterior tibial veins; 3, submalleolar perforator vein; 4,
foot perforator vein; 5, lower posterior tibial perforator vein; 6,
middle posterior tibial perforator vein; 7, higher posterior tibial
perforator vein; 8, medial gastrocnemius perforator vein; AT,
Achillean tributary; CP, calcaneal perforator vein (connected to
the lateral plantar veins); GS, great saphenous vein; SSV, small
saphenous vein.
Perforator veins of the ankle and lower leg
At different levels, horizontal or oblique anastomoses (deep communicating veins) between the posterior tibial, anterior tibial, and fibular veins may be present (Figure 11). These horizontal anastomoses between the three deep veinous axes are not randomly distributed, but located at several levels, which define the hemodynamic levels, explain the fixed location of the leg perforator veins,<sup<8 and allow for venous blood flow exchange when needed.
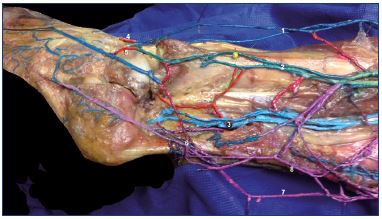
Figure 11. Anatomical dissection of right foot after removing the
fibula (lateral view).
Latex injection. In this image, the three deep venous axes of
the leg are simultaneously shown, with multiple transversal
anastomoses (deep communicating veins).
Abbreviations: 1, anterior tibial veins; 2, fibular veins; 3, posterior
tibial veins; 4, dorsal foot perforator vein to anterior tibial veins;
5, dorsal foot perforator vein to the fibular veins; 6, roots of the
small saphenous vein; 7, Achillean tributary; 8, trunk of the small
saphenous vein.
Hemodynamic characteristics of foot perforator veins
A unique feature for some foot perforator veins is that they are commonly provided with one-way valves to explain their unidirectional flow, from deep to superficial, which is unique in the venous system of the lower limbs. Figure 12 shows the valves present along all of the medial perforator veins, which explains the ascending flow in both saphenous veins during systolic activation of the foot venous pump. In fact, during calf systole, the posterior tibial veins are closed, and the main outlet could only be the two saphenous systems, in particular into the medial marginal vein via the perforator of the first intermetatarsal space. However, it is important that, rather than dividing the foot veins into deep and superficial, the foot veins should be divided into two functional units–medial and lateral.
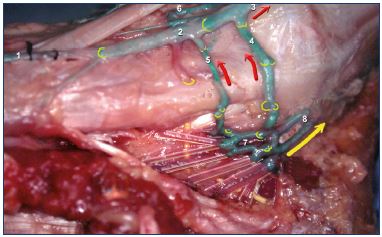
Figure 12. Anatomical dissection of the right foot.Medial
perforator’s valves (medial view).
Latex injection. This image shows confluence (7) plexus of
the plantar veins (not injected) with the origin of posterior
tibial veins (8). The blood is ejected upward in the leg during
plantar systole (yellow arrow), but the deep venous blood is
also injected toward the superficial system (red arrows) via the
medial foot perforator veins inframalleolar perforator vein (4)
and navicular perforator vein (5), where the valves are oriented
from deep to superficial.
Abbreviations: 1, dorsal vein of hallux; 2, medial marginal
vein; 3, great saphenous vein; 4, inframalleolar perforator vein;
5, navicular perforator vein; 6, anterior communicating vein
(origin of the anterior tibial veins); 7, calcaneal confluent veins;
8, posterior tibial veins.
The medial functional unit is comprised of the medial plantar veins, the medial marginal vein, the dorsal perforating vein (or dorsal communicating vein), which gives rise to the anterior tibial vein and all of the medial foot perforator veins–inframalleolar, navicular (or scaphoid), and cuneal. The lateral functional unit is comprised of the lateral plantar veins and the calcaneal perforator vein, which forms the posterior root for the small saphenous vein. Therefore, during the systolic phase of the foot, venous return is shunted when the posterior tibial veins are not open, the blood is pushed up into both saphenous systems, ie, medially into the medial marginal vein, the main root for the great saphenous vein, and laterally via the calcaneal perforator vein, which is commonly connected to the Achillean vein and joins the small saphenous vein in the lower third of the calf.
During contraction of the calf muscle pump, while walking, the passage of blood through the posterior tibial and fibular veins is not possible.10 Consequently, during calf muscle pump systole, venous blood return from the foot must take alternative routes. This goal is achieved thanks to “physiological shunting” through foot perforator veins, from the deep plantar veins toward the superficial veins,11 including both saphenous axes. Outward blood flow through the lower posterior tibial perforator vein (Cockett I) is common in subjects without venous insufficiency, probably accomplishing the same functional purpose. Since foot perforator veins and lower leg perforator veins are located at the lower end of limb’s venous system, ie, below the calf muscle pump, inverted flow during muscle activity should not be interpreted as either abnormal or physiological “reflux,” but as a “physiological shunting.” Real-time ultrasound assessment during provocative maneuvers is a dynamic, noninvasive, diagnostic tool that can show inverted flow through these perforator veins in people without venous disease (Figure 13). Our anatomical data were confirmed with 3D modeling of CT venography data. Figure 14 shows the plantar veins with their connections to the superficial system, particularly the roots for the great saphenous vein.
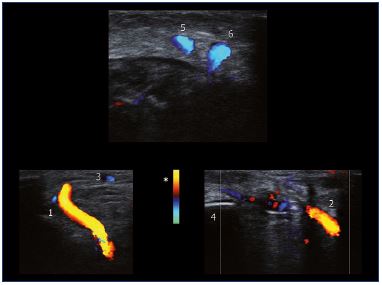
Figure 13. Ultrasound images of the right foot in a person
without venous disease.
Inverted flow through the first intermetatarsal (1) and premalleolar
(2) perforator veins during provocative maneuvers. Flow towards
the probe is coded in red (*). Ultrasound demonstration of
inverted flow within foot perforator veins is a common finding
in individuals without evidence of chronic venous insufficiency.
In the same subject, a transverse scan of the right lower leg
shows flow augmentation through both the Achillean tributary
(5) and the small saphenous vein (6) during foot´s venous pump
systole, which is induced by body weight displacement from the
contralateral limb toward the limb being studied.
Abbreviations: 1, first intermetatarsal perforator vein; 2,
premalleolar perforator vein; 3, superficial dorsal venous arch;
4, lateral malleolus; 5, Achillean tributary; 6, small saphenous
vein.
Images reproduced with permission from Dr Miguel Lo Vuolo.
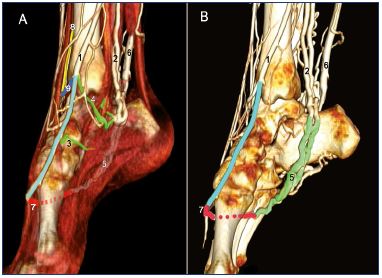
Figure 14. Three-dimensional modeling of medial and lateral
foot perforator veins.
Direct CT venography with the muscles and tendons (Panel A)
and without (only veins and bones) (Panel B).
Abbreviations: 1, great saphenous vein; 2, posterior tibial veins;
3, navicular perforator vein; 4, inframalleolar perforator vein; 5,
lateral plantar veins; 6, small saphenous vein; 7, perforator vein
of the first inter-metatarsal space; 8, anterior tibial vein; 9, dorsal
perforator to the anterior tibial vein.
Clinical consequences
The role of the foot venous pump and foot perforator veins should not be underestimated. Despite the small volume of blood ejected with every step, foot perforator veins play an essential role in the lower limb’s venous return,9 which is the reason why any foot static disorder (flat or hollow foot) will impair the foot venous pump, and the clinical condition of a patient with chronic venous disease could worsen. As shown in our previous study, foot static disorder could be considered a major risk factor for chronic venous disease.12,13 In daily practice, it is mandatory to check for foot static disorder in our patients and correct the problem with an insole, which will improve the symptoms related to chronic venous insufficiency and foot static disorder. In fact, we should keep in mind that about 60% of the so-called venous symptoms do not have a venous origin.14
The clinical consequences of the foot venous anatomy are also interesting because varices of the foot could be related to a zone of weakness at the ankle.15-16 When submitted to a reentry flow caused by a great saphenous reflux, the local venous hypertension is increased by the peaks of pressure created by the foot venous pump systole, and transmitted by the foot perforator veins into the superficial venous system.
Conclusion
Foot perforator veins are characterized by a distinctive feature in the lower limb: the blood can flow from the deep to the superficial veins due to the presence of valveless or “inverted-valve” perforator veins, which act as shortcuts between the foot venous pump and the superficial venous system. During calf muscle pump contraction, these perforator veins shunt the foot´s venous return, which explains the augmentation in systolic flow that is observal in both saphenous axes.
REFERENCES
1. Uhl JF, Gillot C. Anatomy of the foot venous pump: physiology and influence on chronic venous disease. Phlebology. 2012;27:219-230.
2. Uhl JF, Gillot C. The plantar venous pump: anatomy and physiological hypotheses. Phlebolymphology. 2010;17:151-158.
3. Uhl JF. Three-dimensional modeling of the venous system by multislice helical computed tomography venography: technique, indications and results. Phlebology. 2012;27:270-288.
4. Uhl JF, Verdeille S, Martin-Bouyer Y. Three-dimensional spiral CT venography for the pre-operative assessment of varicose patients. Vasa. 2003;32(2):91- 94.
5. Uhl JF, Caggiati A. Three-dimensional evaluation of the venous system in varicose limbs by multidetector spiral CT. In: Catalano C, Passariello, eds. Multidetector-Row CT Angiography. Spinger Berlin Heidelberg; 2005:199- 206.
6. Uhl JF, Ordureau S. New computer tools for virtual dissection to study the anatomy of the vascular system. Phlebolymphology. 2008;15(4):151-155.
7. Uhl JF, Plaisant O, Gillot C, Martin- Bouyer Y, Verdeille S. Virtual reality in anatomy: value and limitations. Surg Radiol Anat. 1998,20:76.
8. Uhl JF, Gillot C. Embryology and threedimensional anatomy of the superficial venous system of the lower limbs. Phlebology. 2007;22(5):194-206.
9. Gardner AM, Fox RH. Peripheral venous physiology. In: Gardner AM, Fox RH, eds. The Return of the Blood to the Heart. London: John Libbey; 1993:61-87.
10. Lo Vuolo M. Venous Ultrasound: a Comprehensive Approach. Lower Extremities and Pelvis. 2014.
11. Pegum JM, Fegan WG. Anatomy of the venous return from the foot. Cardiovasc Res. 1967;1:241-248.
12. Uhl JF, Chahim M, Allaert FA. Static foot disorders: a major risk factor for chronic venous disease? Phlebology. 2012;27(1):13-18.
13. Saggini R, Bellomo RG, Iodice P, Lessiani G. Venous insufficiency and foot dysmorphism: effectiveness of viscoelastic rehabilitation systems on veno-muscle system of the foot and of the calf. Int J Immunopathol Pharmacol. 2009;22(suppl 3):1-8.
14. Uhl JF, Chahim M, Allaert FA. Compression versus inner sole for venous patients with foot static disorders: a prospective trial comparing symptoms and quality of life. Phlebology. 2015;30:32-38.
15. Ricci S, Moro L, Antonelli Incalzi R. The foot venous system: anatomy, physiology and relevance to clinical practice Dermatol Surg. 2014;40(3):225-233.
16. Ricci S. The venous system of the foot: anatomy, physiology, and clinical aspects. Phlebolymphology. 2015;22(2):64-75.