Diagnosis, Investigations, Management, and Progression
Keynote lectures
Clinical implications and diagnostic applications of hemodynamic measurements
in chronic venous disease
Andrew Nicolaides (Cyprus)
Venous hemodynamic concepts are useful in understanding the pathophysiology of venous disorders, the significance of investigation results, the hemodynamic changes associated with symptoms, and the hemodynamic changes associated with treatment. Hemodynamic measurements of pressure, volume, pressure/volume relationship, velocity, flow, resistance, compliance/elasticity, function of the calf muscle pump, and changes in the microcirculation are very important. Unfortunately, only velocity and flow can be measured by duplex ultrasound. Four main phases are observed in the progression of chronic venous disease: valve damage (reflux), vein wall remodeling (varicose veins), capillary leakage (edema), and capillary damage (skin changes). Venous hypertension is the underlying hemodynamic change associated with the increased prevalence of skin changes and ulceration. However, there are protective mechanisms, such as lymphatic drainage and fibrinolytic activity. Lymphatic drainage can increase 5 to 10 times in some individuals, but only 2 times in others and 0 in patients with lymphedema. In the presence of moderate venous hypertension, if the fibrinolytic activity is low, 90% develop skin changes and 70% develop ulcers; however, if the fibrinolytic activity is normal or high, only 16% develop ulcers. For quantitative measurements of reflux in individual veins, volume flow can be measured using duplex ultrasound (time average velocity x vessel cross-sectional area = rate of volume reflux in mL/min). For whole leg measurements, air-plethysmography can be used. In patients with venous obstruction, the degree to which a venous stenosis is critical is not known because outflow resistance depends not only on the degree of stenosis, but also on the degree to which the collateral circulation is developed. Resistance can be measured from simultaneously obtained outflow curves of pressure and volume (R=P/Q). When reflux and resistance are measured, there is a high correlation between these combined measurements and the venous clinical severity score. Therefore, the statement that “there is a poor correlation between hemodynamic measurements and the clinical severity of chronic venous disease” should be modified to “there is a poor correlation between duplex measurements and the clinical severity of chronic venous disease.” Duplex measurements provide information on the presence or absence and anatomic extent of reflux or obstruction. If quantitative information is needed for how much reflux or obstruction exists for clinical decisions, duplex measurements should be complimented with plethysmography.
Changing concept on venous hemodynamics: contemporary interpretation!
Byung-Boong Lee (USA)
Lee addressed the contemporary interpretation of Cockett’s blow-out syndrome. Despite the many excellent guidelines for clinicians on the management of venous disorders, the hemodynamic background of venous disorders has rarely bee reviewed seriously as an independent issue. Therefore, the hemodynamics of the venous system is largely unexplored, not at all understood, and the available models have been shown to be inadequate. Indeed, the hemodynamic concepts involved have remained unchallenged through recent decades mainly due to their complicated nature. However, the development of duplex scanning and other imaging techniques with outstanding resolutions that can provide information on the anatomic extent of reflux and obstruction have become a mainstay for the diagnosis and clinical decisions without an in-depth understanding of the background hemodynamic processes involving flow, pressure, compliance, and resistance. Based on tremendous improvements in the diagnostic technology, physicians can understand many difficult conditions/phenomena better.
The term “competent calf perforator” is misleading; the division into “competent” and “incompetent” calf perforators is arbitrary, freely contrived, and unjustified (Rozhl Chir. 1973;52:142). Lower leg perforators do not function in healthy people as a competent, one-way system. Pressure recordings in the posterior tibial veins and great saphenous veins show both unhindered pressure transmission in either direction within the calf perforators and prompt systolic and diastolic pressure equalization both in patients with varicose vein and large “incompetent” perforators and healthy people with “normal” perforators. Therefore, deep and superficial veins of the lower leg form conjoined vessels to maintain a “physiological” bidirectional flow. The outward flow in calf perforators is not reflux; the reflux is a diastolic, centrifugal, pathological flow within the calf perforators with inward-oriented flow into deep lower leg veins inducing ambulatory venous hypertension. The outward flow is a systolic, centripetal flow that is propelled by the calf pump via the great saphenous vein in the physiological direction of the heart. The calf pump has a double-barreled outflow, with the main flow being through the popliteal-femoral axis and the second flow through the great saphenous vein. Simultaneous pressure recordings in the posterior tibial veins and the great saphenous vein showed that calf perforators provide free pressure transmission between deep and superficial veins of the leg, resulting in quick pressure equalization. These findings indicate that deep and superficial veins of the lower leg form conjoined vessels to meet physiologic needs.
Innovations in the treatment of varicose veins
The new Latin American therapeutical guidelines in the treatment of chronic venous insufficiency
Roberto Simkin (Argentina)
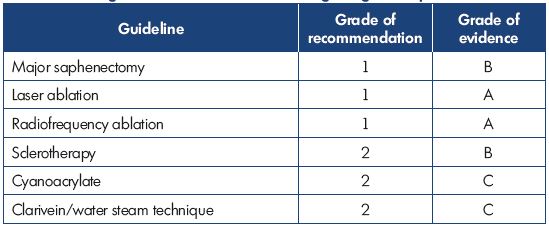
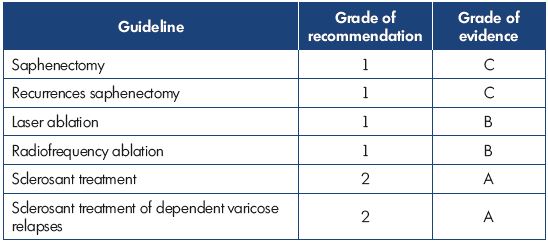
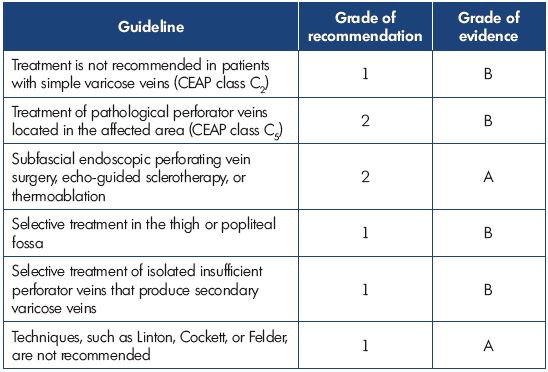
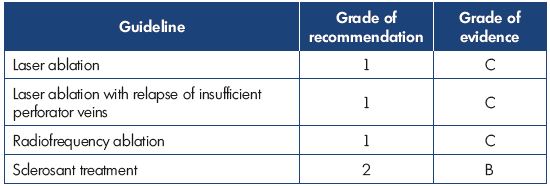
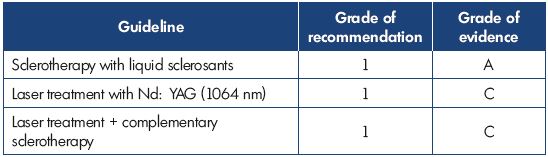
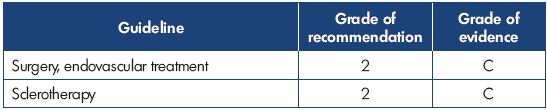
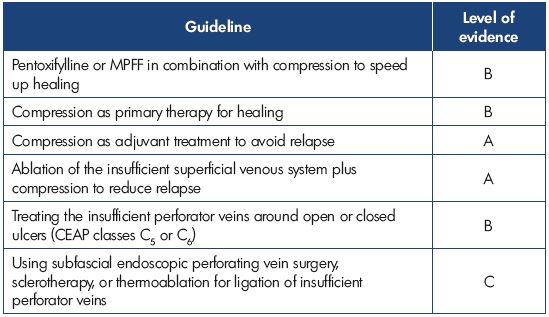
Dr Simkin presented an overview of the recently published Latin American guidelines on the management of chronic venous insufficiency. For grading of the recommendations and quality of evidence, the grading scheme GRADE, which was formulated by the American College of Chest Physicians (ACCP) and published in Chest in 2006, was used. This grading scheme classifies recommendations as strong (grade 1) or weak (grade 2), according to the balance of and the degree of confidence in the benefits, risks, burdens, and possibly cost. The system classifies the quality of evidence as high (grade A), moderate (grade B), or low (grade C) according to factors that include the study design, consistency of the results, and directness of the evidence. The Latin American guidelines were adapted to the socioeconomic reality of Latin America countries. The following tables show the results for treating the great saphenous vein (Table I), the small saphenous vein (Table II), insufficient perforator veins (Table III and Table IV), telangiectasias and reticular veins (Table V), symptomatic relapsed varicose veins (Table VI), and venous ulcers (Table VII). Simkin pointed out that these guidelines do not intend to be a dogma and they should be used with the experience of the treating specialists and the preferences of the patients.
Compression therapy during EVLA of the GSV
Ruben Velletaz (Argentina)
In a randomized controlled study that evaluated the effect of compression therapy after endovenous laser ablation of the great saphenous vein showed that neither graduated compression stockings nor concentric compression bandages could achieve adequate compression of the thigh while standing. In the clinical guidelines for the diagnosis and management of varicose veins from the National Institute of Clinical Excellence, no clear recommendations about the type and duration of compression therapy after endovenous laser ablation have been determined. The primary objective of this study was to establish a compression therapy protocol. The patients were randomized into two parallel groups: (ii) group 1 (n=98) received conventional compression therapy with high extension bandages 0 to 7 days postprocedure; and (ii) group 2 (n=76) received eccentric compression 0 to 2 days postprocedure. After day 7 or 2, respectively, both groups received graduated compression stockings (20 to 30 mm Hg) until day 14. The following outcomes were assessed: clinical scores (CEAP, VCSS), quality of life (CIVIQ 20), adherence to compression therapy, pain (VAS), tolerability, and safety parameters. The patients in group 2 had a lower pain intensity, lower analgesic intake, lower rates of side effects (ecchymosis, induration, and pigmentation), a lower rate of progression of endothermal heat-induced thrombosis, and a higher quality of life score than did the patients in group 1. In conclusion, in terms of pain intensity, tolerability parameters, and quality of life, eccentric compression for the first 2 days after endovenous laser ablation of the great saphenous vein followed by graduated compression stockings for 14 days is superior to compression therapy with high extension bandages for 7 days followed by graduated compression stockings for 14 days.
Telangiectasia: etiological classification and combined synergic treatment
Carlos Simkin (Argentina)
According to the consensus statement from the Latin American Venous Forum, telangiectasias are classified as primary or secondary on an etiologic point of view. Telangiectasias was further subdivided into those with a high response, a good to moderate response, and a low to poor response depending on their behavior in front of the light impact and therapeutic effect obtained. In his daily practice, Simkin combines transdermal cryolaser (Nd:YAG [1064 nm]) with cryosclerotherapy (0.5% liquid polidocanol and a 50% glucose hypertonic solution mixed with 0.33% sodium tetradecyl sulfate) to treat telangiectasia and reticular veins. This combination treatment should result in a synergistic effect between the chemical effect of sclerosis, the physical effect of the laser, and the anesthetic and local anti-inflammatory effect of the cryotherapy. In Simkin’s opinion, transdermal cryolaser is indicated when conventional sclerotherapy is not effective, in patients with a needle phobia, when patients would like a new treatment, in the case of an allergy to the sclerosant agents, when the patient is taking anticoagulants, and when the patient is breastfeeding. Contraindications for cryolaser include Raynaud phenomenon, autoimmune diseases, peripheral occlusive arterial disease, laser phobia, and certain skin diseases (pemphigus, psoriasis).
Simkin reported on his 10 years of clinical experience. Of the 7964 patients treated with cryolaser and cryosclerotherapy between 2001 and 2012, 20% received cryosclerotherapy, 22% cryolaser, 41% cryolaser plus cryosclerotherapy, and 17% cryolaser plus cryosclerotherapy plus microsurgery. Complications after cryolasertreatment included skin burns (0.26%), hyper/hypopigmentation (0.7%), hematoma and ecchymosis (6%), and localized intravascular coagulation (11%). Therefore, Simkin concluded that the combination treatment with cryolaser and cryosclerotherapy was more effective and faster acting than monotherapy. In trained hands, the combination of transdermal cryolaser associated with cryosclerotherapy is a good technique with excellent esthetic and clinical results, high patient satisfaction, and a low rate of complications.
Klippel-Trenaunay syndrome: treatment with endovenous laser. Long term results with the regional segmentary skeletonization technique
Roberto Simkin and Carlos Simkin (Argentina)
Klippel-Trenaunay syndrome presents with atypical varicose veins, diffuse angiomas, arteriovenous fistulas, pigmentary nevus of variable sizes and length on the extremities. There are three types of surgical management for this disease, including vein resection, regional segmentary skeletonization (named the Simkin technique), and endoluminal laser. Eight cases were treated with a hybrid technique, which consisted of treating the junction and the saphenous veins with the endoluminal laser technique (980 nm), and treating collateral veins, perforator veins, and vulvar veins by resection, cryolaser (540 nm), or foam sclerotherapy. In conclusion, regional segmentary skeletonization is a good technique for reducing the abnormal growth of the affected extremities, and the endoluminal laser technique is a good choice for treating recurrent varicose veins in patients with Klippel-Trenaunay syndrome.
Evaluation of CVD patients: from CEAP to symptoms
Introduction
Lowell S. Kabnick (USA)
Kabnick thanked the International Union of Angiology for bringing the American Venous Forum and the European Venous Forum together to discuss the session’s topics. He expressed his expectations on controversy and disagreement. He also posed several questions to think about, such as “how reliable are symptoms in predicting venous disease and severity” and “what are the benefits and the issues of the CEAP classification,” and “do we really need to revise.” Finally, Kabnick congratulated the authors of the SYM Vein Consensus statement that was developed under the auspices of the European Venous Forum.
Do venous symptoms tell all?
Michel Perrin (France)
Perrin explained why venous symptoms provide few or even false information on patients status. One reason is that leg symptoms are not pathognomonic of venous disease (except venous claudication), and venous disease can be asymptomatic, and there is a weak correlation between symptom intensity and severity of the venous disease. However, secondary symptoms, such as disquiet, malaise, insomnia, illbeing, etc, may be related to a venous disease, but this relationship might be difficult to establish. There is also a weak correlation between symptom intensity and the information drawn from the instrumental investigation; some patients obtain symptom relief with any treatment (ie, the placebo effect). Another factor is that the perception of symptoms is individual, and consequently, the patients’ self-reported information on symptoms is not valuable in the assessment of symptom severity. While venous symptoms provide physicians with important information, the symptoms do not reflect the pathophysiologic disorders that affect the venous system: reflux, obstruction, or both. From June 2014 to June 2016, 23 participants from 14 countries agreed to work together to clarify some of the problems raised by the issue of venous symptoms. Five groups were formed to deal with five major topics: description and definition of venous symptoms; attributing leg symptoms to venous disorders; pathophysiology of venous symptoms; venous symptom scoring, clinical examination, and instrumental investigations. The results of this work were published as the SYM Vein Consensus statement (Int Angiol. 2016;35:374-398). Perrin concluded that this consensus document helps with many issues, but many points remain to be clarified.
Venous symptoms: what are they and how can we be certain?
André van Rij (New Zealand)
Venous symptoms are related to different venous problems, such as thrombosis, reflux, obstruction, perforator dysfunction, phlebitis, varicose veins, skin manifestations, recurrence, and ulcers. There is the dilemma regarding the lack of specificity, frequency, overlap, variety in intensity, and lack of correlation between these symptoms and pathology, and as a result, there could be a high treatment bias. van Rij suggested how to attribute symptoms to venous disease: (i) the human factor should be understood, which consists of many psychosocial and individual factors; (ii) the symptom story has to be interrogated and established; (iii) the probability of association needs to be known, other causes should be excluded, and symptoms should be related to signs/investigations; and, finally, (iv) the response to conservative therapy has to be evaluated.
History of CEAP: past and present
Bo Eklof (Sweden)
A classification of chronic venous disease is needed because it is fundamental to the understanding of the clinical disease processes and communication between institutions. There have been many published classifications of chronic venous disease; the first classification was published by Widmer in 1978, and it distinguished between stage I (edema and dilated subcutaneous veins with corona phlebectatica), stage II (trophic lesions of the skin with hyperpigmented or depigmented areas), and stage III (healed or active venous ulcers). The problem with the old classification systems is that, because venous disease is complex, the clinical diagnosis is not enough, as it provides no information about the etiology, anatomy, and physiology of the disease. In 1993, the need for a better classification was discussed at the American Venous Forum, and as a result, an ad Hoc Committee of the American Venous Forum developed a new “Classification and Grading of Chronic Venous Disease in the Lower Limbs.” This “CEAP” classification was based on 4 points: (i) what: Clinical manifestation; (ii) why: Etiologic basis; (iii) where: Anatomic distribution; and (iv) how: Pathophysiology. This classification was distributed over 5 continents with 26 publications and 11 language translations.
Further improvements to the CEAP classification concerning the definition of C were made at the International Union of Phlebology meeting in 2001. The suggested definitions and refinements of C in CEAP were published in the Journal of Vascular Surgery in 2003. By 2004, an ad hoc committee to review the CEAP classification and make recommendations for change was established. The main points of the revision included a refinement in the definitions used to describe chronic venous disease, a refinement of the C classes, and the addition of the descriptor n. The revision also defined levels of investigation: (i) Level I: office visit with history and clinical examination; (ii) Level II: noninvasive vascular lab; and (iii) Level III: invasive investigations or complex imaging studies. Besides the revision, Eklof introduced basic CEAP with the use of the single highest descriptor for the C class vs the advanced CEAP where the use of all of the components is encouraged. The revision of the CEAP classification was published in the Journal of Vascular Surgery in 2004, and now a new revision is planned in collaboration between the American Venous Forum and the international phlebology community.
What are the benefits of CEAP?
Ruth Bush (USA)
Bush discussed the CEAP classification from different points of view. For the practicing physician, CEAP can be an instrument to diagnose the disease correctly, guide the treatment, and assess the prognosis. For reporting standards and researchers, CEAP should be a descriptive instrument to categorize patients into different groups of chronic venous disease severity. Bush pointed out that a proper diagnosis and accurate classification of the underlying venous problem is the cornerstone for the management of chronic venous disease; however, there is heterogeneity in the reporting standards concerning demographics and outcomes.
In a medical database search, which was conducted by Thakur et al and published in Eur J Vasc Endovasc Surg in 2010, randomized clinical trials published between 1968 and 2009 that evaluated endovenous interventions for varicose veins were included, and the trial details were compared with the recommended reporting standards published by the American Venous Forum in 2007. From 2384 identified abstracts, only 28 randomized trials fulfilled the inclusion criteria, and there were wide variations in both the reporting and the assessed outcome measures. Meaningful comparisons were difficult due to variations in the study design, the lack of quality of life data, and the lack of comparison to published reporting standards. The only good news was that demographic reporting improved after 2007. The CEAP revision includes more detail on severity, pathology, and anatomy; the CEAP classification is not a static classification and revision is an ongoing process. CEAP represents the clinical and functional situation of the patient, but not disease severity. In a trial published by Kahn et al in 2004, the clinical category, based on CEAP classification, predicted patients reported quality of life and symptom severity in chronic venous disease.
Some of the advantages of the CEAP classification include assisting in the evaluation of various treatment modalities, allowing results from multiple institutions to be compared, enhancing the understanding of the potential etiologic factors and the pathogenesis of the disease, and improving the scientific standards of the published literature. A standardized approach for assessing the outcomes helps minimize the number of expensive and lengthy prospective randomized trials, improves practice audits, and assists in registry data acquisition. Finally, Bush introduced the Varicose Vein Registry (VQI) that was launched in January 2015. To date, 13 countries have reported data on 826 patients and 844 limbs from the first 6 months. In conclusion, considerable variation exists in study populations and outcome measures; therefore, randomized trials should adhere to reporting guidelines and agreed upon standards, which will allow for greater objectivity when assessing new technologies. Bush marked CEAP as very beneficial, and she recommends using the basic CEAP for daily practice and the full CEAP for scientific use.
What are the issues with CEAP?
Pier-Luigi Antignani (Italy)
CEAP remains the gold-standard classification for chronic venous disease, which was confirmed in a recent review article where the authors conducted a Medline analysis that retrieved 266 publications using CEAP. The CEAP classification has limits because it is not a severity classification and the classes C0 to C3 are controversial. The C0s patient condition was the true problem in clinical practice because the majority of people classified as C0 (20% of general population) were symptomatic (C0s). Antignani stressed that venous disorders are individual-based pathologies and patient satisfaction becomes a hallmark of effective treatment. Then Antignani pointed out that the CEAP classification and venous clinical severity score (VCSS) are different tools that do not measure the same items equally. For example, C2 uses a definition of >3 mm for a varicose vein, whereas the VCSS uses a cut-off point of 4 mm. In Antignani’s opinion, the major handicap of CEAP is its complexity, which makes it difficult to use in everyday practice. Other limitations include the lack of general information provided (ie, patient history), the lack of reversibility of language (eg, C4 means, at the same time, one or several skin changes), the lack of a varicose vein score, the fact that C2 summarizes all kinds of varicose veins, separating venous and other cause of edema in the C3 class may be difficult, and corona phlebectatica of the foot is not taken into account, which is classified as a strong clinical predictor of chronic venous disease and the subsequent occurrence of skin changes. Corona phlebectatica has been identified as a highly significant clinical sign indicating chronic venous insufficiency. It has prognostic value for the progression of chronic venous disease, and it should be evaluated in every patient with chronic venous disease. Antignani proposed that corona phlebectatica be considered for inclusion in existing or future classifications/scoring of chronic venous disease.
The future of disease classifications and the impact of classification change
Fedor Lurie (USA)
Lurie explained the three different types of classifications: clinical classification, research classification, and demographic/descriptive health statistics classification. They differ radically due to different goals, development, basis, reliability/repeatability, responsiveness, and convenience/practicality. For example, demographic/ descriptive classifications, such as CEAP, have a goal of defining distinct diseases and conditions, they are on a phenotype basis after empiric development, and they have high reliability/repeatability; however, responsiveness is not important, and convenience/practicality is low. The big challenge in working out classifications is disease heterogeneity. One possible solution includes merging clinical and research classifications, but this requires knowledge of the pathologic mechanism or molecular etiology. Another solution includes increasing the discriminatory precision of clinical classification, which requires knowledge of the phenotypic variations of mechanismbased subtypes.
Lurie also showed some effects of changing descriptive classifications; for example, after introducing the new classification on the analysis of respiratory mortality trends in England and Wales, the number of deaths assigned to the respiratory disease decreased by 22%. In a publication comparing two scoring systems for injury mortality, it was shown that changing classifications could affect the ranking of the causes of injury mortality, with consequences for public health policy. A study was presented dealing with human disease classification in the postgenomic era and with a proposed complex systems approach to human pathobiology, published in Molecular Systems Biology in 2007, where the authors stated that the contemporary classification of human disease has significant shortcomings as there is a lack of sensitivity in identifying preclinical disease and a lack of specificity in defining disease unequivocally. Lurie classified CEAP as a descriptive classification, where there is insufficient knowledge for a true clinical or research classification, and revisions will result in an additional time delay for evidence synthesis. Improvements in a descriptive classification do not serve the general trend toward a mechanistic classification of diseases.
Chronic venous insufficiency: different viewpoints?
Unusual etiology of recurrent varicose leg ulcer
Georges Tabet (Lebanon)
Six clinical cases of patients with posttraumatic arteriovenous fistula presenting with recurrent leg ulcers simulating varicose leg ulcers were discussed. Most of the patients had a delayed correct diagnosis and treatment, sometimes even for decades. Chronic leg ulcers may be the only symptom of a large posttraumatic arteriovenous fistula in young adults, but varicose leg ulcers are more frequent in the elderly. Other symptoms of an arteriovenous fistula could be congestive heart failure, varicose veins due to venous hypertension, skin pigmentation with or without eczema, and distal ischemia. The femoral artery is most often affected. Patients with an arteriovenous fistula are usually asymptomatic on presentation, and 30% to 70% had a delayed diagnosis. The late complications include arterial and venous dilatation, distal ischemia, venous congestion, and congestive heart failure. In the discussion, the surgical treatment of arteriovenous fistula involving control of arteries and veins above and below the fistula was mentioned, and a distinction was made between endovascular techniques by use of stent-graft coverage with embolization and open repair of the fistula. In conclusion, an accurate history, including any history of trauma in addition to standard examinations (clinical presentation, duplex investigation), should be carried out in patients with leg ulcers. Rare causes for leg ulcers should also be kept in mind to avoid disadvantages for the patients.
Which evaluation criteria for recurrent superficial venous insufficiency?
José Maria Escribano (Spain)
Varicose vein recurrence could reach 80% at the 10-year follow-up. These recurrences may be caused by surgical techniques (20% to 30%), a progression of the underlying disease, or neovascularization. The possible mechanisms involved in the development of recurrences include (i) “in situ” junction (12%), which was often due to a faulty surgical technique; (ii) neojunction (6%); (iii) cavernoma with stump (31%); (iv) cavernoma without stump (20%); cavernoma of the fossa poplitea (8%); and (v) telangiectasia after surgery (72%). Classification of recurrences was presented related to surgical inaccuracies: (i) class A: default closing of the escape point; (ii) class B: drainage failure; and (iii) class C: the emergence of a new leak point. In conclusion, the majority of recurrences follow a defect in the closure of the escape point, which is linked to a technical error, but some recurrences, such as pelvic shunts, are technically difficult to prevent.
Minimally invasive procedure for pelvic leak points in women
Roberto Delfrate (Italy) and Claudine Hamel-Desnos (France)
Between January 2003 and August 2016, the incidence of inguinal and perineal leak point treatment in women was as high as 9.2% of all surgical treatments in Delfrate’s department. The diagnosis in all patients was performed by duplex scan according to the anatomic, functional findings and systematization published by Claude Franceschi. Minimally invasive surgery was used on an outpatient basis under local anesthesia. A total of 250 surgical procedures with at least a 1-year follow-up were performed. Among all of the controlled pelvic leak points, no reflux redo was detected in 98% of the procedures, and no major complications occurred. Taking into separate consideration each pelvic leak point, the recurrence rate was 1.8% for the perineal point, 1.13% for the inguinal point, and 25% for the clitoridian point. These results show that a minimally invasive surgery for reflux with pelvic origin is possible. While the recurrences are low for the inguinal point and perineal point treatment, they are high for the clitoridian point.Therefore, accurate ultrasound assessment of each specific pelvic leak and a specific surgical technique are the keys for satisfactory outcomes.
For Hamel-Desnos, she treats perineal and vulvar varices by first conducting a pretreatment assessment that includes a clinical assessment and a duplex ultrasound of the iliac veins, lower leg veins, and perineal and vulvar varices. If there is no pelvic congestion syndrome and suspected pelvic or suprapelvic obstruction, sclerotherapy of varicose veins is done. Hamel-Desnos recommended using foam sclerotherapy, stretching the skin, and gently puncturing the vein, but she did not recommend using alcoholic solutions for vulvar asepsis. In conclusion, if there is no obstruction or pelvic congestion syndrome, she recommended sclerotherapy for pudendal and vulvar varices. In the case of a doubtful pelvic congestion syndrome, obstruction, or very large varices, further investigation and eventually embolization should be performed.
Complex chronic limb edema: a practical approach
The concept of complex chronic limb edema
Christine Moffatt (UK)
Moffatt explored the different types of patients suffering from chronic edema, discussed the difficulties in establishing the size and impact of the problem worldwide, introduced emerging evidence that chronic edema is a major public health problem, described an international response to the lack of epidemiology (LIMPRINT), and explored the results of the LYMPHORAC study that examined the cost of care to patients. Chronic edema is predicted to increase substantially due to demographic changes, such as an increasing elderly population, increasing obesity, decreased mobility, and the association with cancer and long-term conditions. Approximately 140 to 250 million people worldwide and about 3% of the western population are affected with chronic edema. Chronic edema has a major financial impact in Europe. If chronic edema is treated early and properly, the health care costs could be reduced from 36.3 to 16.5 million euros annually, which is especially important when treating elderly patients (>80 years old) where the costs are 3 times greater than patients aged 65 to 74.
Edema is defined as the presence of abnormally large amounts of fluid in the intercellular tissue spaces of the body. Chronic edema is defined as chronic swelling lasting longer than 3 months that is not resolved by elevation or diuretics. Lymphedema is defined as a chronic, permanent swelling of a whole or part of a limb due, at least in part, to interstitial fluid accumulation and related damage to the lymphatic system and it can be subdivided as either primary or secondary. Moffatt stressed the importance of determining the correct diagnosis and reported that 70% of UK patients have no diagnosis or an incorrect diagnosis. The difficulties are due to the lack of an internationally validated method of classification. In primary care, different types of patients are seen, eg, patients with lymphovenous leg ulcers, obesity, immobility, chronic heart failure, complex chronic illness, and palliative patients. In a prevalence study conducted by Moffatt et al in southwest London in 2003, 833 patients had chronic edema in a population of 619 100. In a prevalence study in Derby City in 2013, 984 patients with chronic edema were identified in a population of 246 900. The difference in prevalence between these two studies in England was statistically significant, which can probably be explained by the different age/sex structures and identification through different specialists; however, a real difference in prevalence cannot be excluded. In the trial in Derby, 17% of the patients had primary chronic edema, 82% had secondary chronic edema, 31% had cancer, 67% had no cancer, and 2% had chronic edema and cancer, and 69% were obese or morbidly obese.
Subsequently, the LIMPRINT study, an ongoing international epidemiology study designed to define the size and impact of patients with chronic edema internationally, was introduced. The data collected from this study will be the largest epidemiology dataset on chronic edema. The study is assessing the prevalence of chronic edema and wounds in each country, the international profile of prevalence, and the impact of chronic edema on patients, the health care system, and society. The results of this study will contribute to a greater understanding of the deficits in health care delivery and provide information on reimbursements. The core tool of the trial that will be used for all patients and in all settings was validated through an international consensus and translated into different languages, and it included five modules: (i) demographics and disability; (ii) quality of life; (iii) details of swelling; (iv) wounds; and (v) cancer. Nine countries–Australia, Canada, Denmark, France, Ireland, Italy, Japan, Turkey, and the UK–are involved in the study.
Complex chronic limb edema: clinical implications and medico-economic consequences
Isabelle Quere (France) and Christine Moffatt (UK)
Quere presented the preliminary results of the LIMPRINT studies from the UK, Denmark, and France in hospitals. The study included 726 patients, and the prevalence results were as follows: in France, 48% had no chronic edema, 22% had wounds, 19% had chronic edema, and 11% had chronic edema and wounds; in the UK, 50% had no chronic edema, 21% had wounds, 17% had chronic edema, and 12% had chronic edema and wounds; and in Denmark, 40% had chronic edema in the Bispebjerg Hospital and 35% had chronic edema in the Frederiksberg Hospital. Quere also reported the results of a study conducted between 2014 and 2015 that aimed to quantify and analyze the out-of-pocket expenses related to the treatment of lymphedema in France. The initial demographic, clinical, and socioeconomic data was collected from LIMPRINT. Of the expenditures, 33% were due to transport, 26% to medical devices, 13% to nursing, physiotherapy, and drugs, 9% to thermal therapy, and 26% to other expenses; 23% forgo medical care because of the costs. Total expenditures over 6 months were 1346±1320 €, and the total out-of-pocket payments were 506±588 €. In summary, the significant out-of-pocket expenses related to lymphedema treatment in France are mainly due to compression therapy devices and transport. Two ways to see change is by advocating for improved pricing and reimbursement policies and in improving the geographic distribution of reference centers.
Which varicose veins lead to venous ulcers (C6)?
The epidemiological analysis
Eberhard Rabe (Germany)
Patients with varicose veins who have an elevated risk for venous leg ulcers should be selected for early varicose vein ablation. Patients who are at risk include C2 patients with corona periphlebectatica, C4 patients with eczema, lipodermatosclerosis, and white atrophy, and patients with popliteal reflux, obesity, and an ineffective calf muscle pump. Obesity and prolonged sitting must be avoided, and compression therapy is mandatory in patients at risk for a venous leg ulcer.
Importance of venous symptoms
Michel Perrin (France)
Perrin discussed the role of venous symptoms in the identification of patients at risk for developing a venous ulcer. No publication shows that venous symptoms, at any severity or intensity, can identify the patients with this risk. In addition, the international SymVein consensus document on venous symptoms was published in International Angiology in 2016. The aim of the consensus document was to describe and define venous symptoms, specify how these symptoms can be attributed to a venous cause, determine the pathology of the symptoms, establish a score dedicated to the symptoms, and determine which clinical examinations and investigations are useful to link symptoms to a venous cause.
The haemodynamic approach
André van Rij (New Zealand)
van Rij stated that, in severe clinical disease, the measurements of reflux and pressure are frequently abnormal, but the specificity is poor.
Duplex ultrasound: characteristics of disease severity, beyond “reflux”
Marianne De Maeseneer (Netherlands)
De Maeseneer focused on hemodynamic measurements (presence of reflux and its duration, peak reflux velocity, and recirculation index) and venous morphology investigations. Duplex ultrasound offers more possibilities than just looking at the presence or absence of reflux, for instance, it can be used to quantify reflux or visualize the venous anatomy and morphology. The relationship with disease severity should be further investigated to increase our understanding of chronic venous disease, and to refine the selection criteria for treatment, targeting those with the largest risk for chronic venous disease deterioration.
Other anatomical factors: microvenules and perforators
André van Rij (New Zealand)
van Rij presented a study describing the presence of microvalves in the very small veins of the skin, which may be critical to whether skin changes occur with venous insufficiency. The concept may explain why some people with long-standing varicose veins do not develop venous ulcers. In addition, degenerative changes in the network of very small veins in the skin of the leg may be related to the appearance of reticular veins, corona phlebectatica, and venous flares. These degenerative changes occur without varicose veins, but are much worse when they occur together. Valvular incompetence could occur independently in small superficial veins in the absence of reflux within the great saphenous vein, small saphenous vein, and the major tributaries. He has shown that, once there is incompetence in third generation “boundary” microvalves, reflux can extend into the microvenous networks in the skin. These effects are markedly worse in the presence of great saphenous vein or small saphenous vein incompetence. It is possible that degenerative changes with valve incompetency are required in larger proximal vessels and small superficial veins, particularly at the “boundary” valves, for the severe skin changes in venous insufficiency to occur.
What can we learn from ultrasound of the skin?
Alberto Caggiati (Italy)
Currently, ultrasonography is used only to designate the location and pattern of venous lesions; however, modern ultrasound devices provide an excellent morphological evaluation of the cutaneous and subcutaneous layers. Ultrasonography refines the visual evaluation of skin changes in legs with venous disorders, and it may reveal changes that are not highlighted by clinical examination. Some of these changes could require further investigation because they have not yet been explained or described. Accordingly, skin sonography may contribute to a better grading of venous disease severity. In particular, in C2 legs, ultrasound evidence of skin changes should be considered to identify those legs in which varicose veins are more than just a cosmetic problem.
How to detect early skin changes?
Patrick Carpentier (France)
Early clinical detection of skin changes would be a major step forward in the evaluation of patients with chronic venous disease because ulcers occur in the altered skin of the lower limbs, which are preceded by induration, pigmentation, and even corona phlebectatica. Early detection remains an unmet challenge due to the problems with specificity, the variability of measurements, and the difficulty in establishing diagnostic thresholds. Carpentier proposed ankle capillaroscopy as a good and feasible tool for the early detection of microvascular skin changes.
Multifactorial approach for treating leg ulcers
New trends in the epidemiology of leg ulcers
Patricia Senet (France)
The available information on the epidemiology of leg ulcers is insufficient, and the existing data is of variable quality and comes from social, economic, and epidemiologic studies published in the USA and some Northern European countries (Sweden, Germany, and the UK). According to the data, the prevalence of all leg ulcers (not just venous ulcers) is estimated to vary between 0.045% and 0.7%, without a real decreasing trend, although older studies had reported a prevalence of 1%. This prevalence increases with age, reaching 2% to 4% in people over 65 years old. A German study (2010-2012) showed that there was a decrease in venous leg ulcers, but an increase in arterial or mixed leg ulcers, which is similar to data from a Swedish registry. There is a female predominance for leg ulcers (60% to 75%), the average age increased to 70-75 years, and the duration of venous leg ulcers and their relapse rates remain high. According to studies conducted in Germany, Italy, the UK, and the USA, the presence of ulcers over 1 year is registered in 24% to 54% of cases; however, in one-third of patients, the leg ulcer is present for over 2 years. The average size of ulcerations is large (35 to 45 cm2).
Patients with leg ulcers have significant comorbidities because 29% to 45% are obese with a BMI >30 (particularly patients with venous leg ulcers), 60% to 80% have high blood pressure, and 30% to 40% have diabetes. A UK study showed that patients frequently come from modest socioeconomic backgrounds, and leg ulcer etiology is constantly changing. The studies on >30 000 German patients and >1000 Italian patients showed a decreasing trend of venous leg ulcers (45.5% to 55% vs the 60% to 80% observed previously), concomitant with an increase in arterial leg ulcers (15%) and mixed leg ulcers (17.5% to 25%). Mixed ulcers or rare etiology leg ulcers represent 10% to 20% of all ulcers. The changing etiology may reflect a real evolution in the etiology or it may be due to a more accurate diagnosis of the leg ulcer etiology. There are no recent studies published regarding the etiology of venous leg ulcers. The data published in 2010 in the Journal of Vascular Surgery showed a network of deep vein involvement in 47% to 60% of venous leg ulcers (one-third of patients had no known history of deep vein thrombosis) and superficial venous insufficiency in 40% to 50% of cases. The life expectancy of patients with venous leg ulcers is identical to that of the general population.
According to data from large clinical trials and Cochrane reviews, the prognosis for venous leg ulcers is a median healing rate of 100 days; 60% to 80% of venous leg ulcers close after 6 months and 65% to 80% in 1 year; 12% to 50% of venous leg ulcers recur at 12 months; in 80% of cases, the venous leg ulcers are small (area
The costs related to the care of patients with leg ulcers are large and growing, representing about 1% to 2% of the annual health care budget in developed countries. In Germany, the costs related to leg ulcers are, on average, 9570 euros/ patient/year, which is higher if the patient is hospitalized. In Sweden, the median reduction in healing from 160 days to 100 days resulted in a significant decrease in the treatment cost from 4000 euros/patient in 2009 to 2134 euros/patient in 2012. New cell therapies for leg ulcers may seem expensive initially, but later they reduce the healing period, which leads to costs that are comparable with standard therapies.
Quality of life is impaired in patients with leg ulcers. A recent UK study showed that the psychosocial impact of leg ulcers is very high: 24.3% had depression, 17.5% anxiety, and 8.4% suicidal ideas. Leg ulcers are a frequent, severe, and costly pathology that can be improved by a correct and early diagnosis, reducing the time of healing, and preventing complications, especially infections.
Major etiological factors: from scientific data to clinical practice
Philippe Leger (France)
There are many causes of skin trophic disorders (erosions or ulcers) in the lower limbs; the most common leg ulcers are venous leg ulcers, arterial leg ulcers, and mixed leg ulcers. Necrotic angiodermitis is a rare vascular leg ulcer that has well-defined clinical and pathophysiological features; however, it should not be confused with the rarer nonvascular ulcers, leading to genuine problems for diagnosis and treatment. These ulcers can occur in the following pathologies: pyoderma gangrenosum, skin cancers, pressure sores, skin infections (eg, tuberculosis, streptococcal ulcers, ecthyma, and skin leishmaniasis), drug rashes, some immunological diseases (eg, disseminated lupus erythematosus, scleroderma, and periarteritis nodosa), hemopathies, or pathomimias. In these cases, a skin biopsy is mandatory. Many factors influence the rate of healing of these leg ulcers, including malnutrition, some medications, additional local infections, diabetes, etc. The same patient may have a venous leg ulcer, diabetes, malnutrition, and a dysimmune disease; therefore, it is important to look at, identify, and treat leg ulcers starting from the existing algorithms for diagnosis and treatment, and the specifics of each patient. In conclusion, Leger proposed a set of seven questions that clinicians should answer when confronted with a new leg ulcer case: (i) is there a contributing low arterial pressure?; (ii) is there venous hypertension?; (iii) is there a problem of local pressure on the skin?; (iv) is there a secondary or superinfection?; (v) are there any associated factors (diabetes, drugs, etc)?; (vi) are there any nutritional problems?; and (vii) is there an atypical aspect of ulceration (pyoderma gangrenosum, skin cancer, angiodermas, pathomimia)?
Leg ulcer patient pathway: wound healing center
Damien Barcat (France)
Chronic ulcers are a public health problem due to their increased prevalence and incidence and the high costs. In some countries, even France, there are wound healing centers, where patients with chronic vascular ulcers are being cared for and monitored. In France, there are still controversies regarding the internal organization and functional procedures in these centers, the center’s financial support, and the assessment of the results. Due to the increasing number of patients with chronic ulcers and the long and difficult journey of patients from one doctor to another, the number of these wound healing centers should increase in the future, and the different specialists should work as a coordinated team. The results must be quantified and published to obtain an accurate and realistic picture regarding the diagnosis, treatment, prognosis, monitoring, and costs for patients with chronic ulcers. These medical structures must be organized, validated, and financed according to the real needs of each country.
Leg ulcer patient pathway: the wound expert nurse
Patricia Bocquet (France)
The care of chronic ulcers, including leg ulcers, means the intervention of experienced or expert nurses in the field. Expert nurses have a special theoretical and practical education, and they work under the direct coordination of a complex medical team (dermatologist, vascular physician, vascular surgeon, diabetologist, etc). Following a first examination by the doctor, the nurses have an active role in the global evaluation of the healing process (ulcer etiology, factors delaying healing, prognosis), implement the therapeutic plan issued by the medical team, and monitor the patients. They offer support to the different medical teams in the hospitals, for ambulatory patients, or at patients’ homes. They are involved in telemedicine, and they make sure that patients with chronic ulcers have good hygiene. They are also involved in the correct application of topical treatments and use of medical devices for ulcer healing according to the indications. In the future, the role of these expert nurses will increase, leading to a better management and a decrease in the costs of caring for patients with chronic ulcers.
Place of the vascular physician in the management of patients with leg ulcers
Christine Jurus (France)
Vascular physicians who are managing patients with chronic wounds, including those with leg ulcers, belong at the center of a complex medical team, preferably in wound healing centers. The reasons for this are that 90% of chronic leg ulcers have a vascular cause and the physician can establish the etiology of these ulcers by complete functional explorations, both on the arterial and the superficial and deep venous hemodynamics. Following these investigations, the vascular physician will issue a therapeutic strategy adapted to each patient. Nevertheless, the vascular physician must work in collaboration with a multidisciplinary team to improve therapeutic results because the incidence of chronic ulcers of other etiologies (infectious, inflammatory dermatological diseases, neoplasia, etc) is increasing.
Chronic venous disease: varicose veins
Results of the prospective noncomparative study of endovenous laser ablation of the saphenous vein more than 2 cm in diameter
Alexey A. Fokin and Denis A. Borsuk (Russia)
This study aimed to determine if veins larger than 20 mm could be ablated. The authors investigated both anatomic and hemodynamic results. They treated 91 patients with saphenous veins that had a mean diameter of 28}4.5 mm using a 1470 nm laser. In the midterm follow-up (total follow-up time, 157}47 days), there was a 98.9% occlusion rate. For this procedure to be successful, it is important to place the fiber in the center of the vein lumen.
Surgical procedure for incompetent perforators: VANST technique
Valerian Ciubotaru (Romania)
The VANST technique (Varices’ Ambulatory Non-stripping Surgical Therapy) relies on the assumption that excluding the failing perforators would eliminate the need for ablating the saphenous vein. The procedure necessitates the mapping and ligation of the failing perforators. A 5-year follow-up of 1279 cases revealed that recurrence occurred only in 89 of the cases. This approach can be applied to a great spectrum of cases, such as axial insufficiency of the great saphenous vein and the small saphenous vein, CEAP classes with more than 4 varicose veins, and recurrent varicose veins. It also obviates the need for postoperative compression, provides minimal invasiveness, and it has ambulatory advantages.
Intraoperative sonography in open venous surgery
Simon Julinek (Czech Republic), Ivan Maly, and Daniela Klein
Intraoperative sonography facilitates the location of optimal puncture sites, determines the diameter of the saphenous vein, assists in the application of a tumescent solution during endovenous surgery, and helps find the tip of the stripper during high ligation of the saphenous vein with local anesthesia. It also protects the surgeon from accidentally treating the sufficient great saphenous vein instead of an incompetent accessory saphenous vein.
Vascular gel model for central venous catheterization
Pongpol Sriphan (Thailand), Piyanut Pootracool, Wiwat Tirapanich, Sopon Jirasiritum, Surasak Leela-Udomlipi, Suthas Horsirimanont, and Nutsiri Kittitiratong
The aim of the study was to develop a homemade vascular gel model for an ultrasound-guided puncture that would be comparable to the standard phantom model to lower costs. The first phase of the study was to develop a homemade gel model. The second phase of the study was to compare the gel model with the standard phantom model used for trainees. The images obtained using the homemade gel models were of high-reliance quality and similar to the standard phantom model, and the gel model is cheaper due to the easy preparation using readily available materials.
An investigation of the relationship between exercise, range of ankle joint movement (ROM) and venous leg ulcer (VLU) healing
Omar Mutlak (UK), Mohammed Aslam, and Nigel Standfield
Mutlak reported the results on the relationship between exercise, the range of ankle joint movement, and venous leg ulcer healing. Two groups of patients were compared: group 1 (n=20) performed exercise only at home and group 2 (n=20) performed exercise at home in combination with compression therapy (short-stretch bandages). The range of ankle joint movement and ulcer size were assessed at baseline and after 3 months of regularly conducted exercises (10 dorsiflexions per hour). At the end of the study, the range of ankle joint movement increased significantly in both groups to the same extent compared with baseline, and ulcer size decreased to a greater extent in the compression group. In conclusion, exercising regularly at home increased the range of ankle joint movement, and it may play a positive role in ulcer healing in patients with venous leg ulcers.
A body weight transfer manoeuvre with minimal ankle movement significantly outperforms the tip-toe manoeuvre in assessing calf muscle pump function
Christopher R. Lattimer (UK), Evi Kalodiki, Claude Franceschi, and Fausto Passariello
This prospective study analyzed the body weight–transfer maneuver with minimal ankle movement vs the tiptoe maneuver on calf muscle–pump function. Three different pumping performances were tested with air-plethysmography: 3 tiptoe movements, 3 ankle dorsiflexion, and 3 body weight–transfer maneuvers. The results showed higher pump efficiency after weight transfer (60%) compared with tiptoe (43%) and dorsiflexion (38%). The isometric weight transfer maneuvers have a better pumping action than ankle maneuvers. Walking exercises should be recommended for patients with chronic venous disease rather than just ankle movements.
Utilising gravitational manoeuvres with a tilt-table to assess a gravitational disease
Christopher R. Lattimer (UK) and Erika Mendoza
In this presentation, the results of a study on gravitational maneuvers on the tilt-table for assessing the effect of gravity on chronic venous disease were reported. The study aimed to quantify gravitational venous drainage in three Trendelenburg positions (standing, reclining, and head down) in 3 groups of 11 patients (healthy, patients with venous obstruction, and patients with venous reflux). Air-plethysmography calf volume changes were continuously recorded. The results showed that gravitational maneuvers on a tilt-table and venous drainage index could be used as noninvasive screening for obstruction, selection for stenting, and stent monitoring.
Correlation between reflux volume of the great saphenous vein and severity of chronic venous disease in patients with primary varicosities Kirill Lobastov
(Russia), A. Vorontsova, A. Bargandzhiya, Victor Barinov, Leonid Laberko, Valeriy Boyarintsev, and Grigoriy Rodoman
Lobastow presented the results of a study correlating reflux volume of the great saphenous vein and severity of chronic venous disease in patients with primary varicosities. In this observational cross-sectional study, 80 patients underwent duplex ultrasound investigations where reflux volume was measured, and both clinical and quality of life parameters were assessed. There was a significant weak correlation between reflux volume and clinical, etiology, anatomy, pathophysiology (CEAP) class, venous clinical severity score (VCSS), and quality of life scores (CIVIQ, VEINESS). The reflux volume was significantly higher in the most severe classes.
Results of endovenous radiofrequency thermal ablation with and without high ligation in comparison with high ligation and stripping in for treatment of great saphenous varicose veins
NS Abushov (Azerbaijan), EJ Zakirjayev, MM Karimov, ZM Aliyev, FE Abbasov, and GN Abushova
In this nonrandomized, observational study, 166 patients were divided into 3 groups and evaluated (75 to high ligation and stripping; 61 to endovenous radiofrequency thermal ablation without high ligation, and 30 to endovenous radiofrequency thermal ablation with high ligation). The patients receiving endovenous radiofrequency thermal ablation with or without high ligation could return to habitual activities earlier, and they had a painless postprocedure period and a better cosmetic effect compared with patients receiving high ligation and stripping. High ligation and stripping should only be used in selected patients with a large great saphenous vein diameter, a proximal aneurysm, and/or superficial thrombophlebitis.
Early patency and feasibility of cutting balloon treating central vein stenosis in hemodialysis patients
Jakchai Boonyavanich (Thailand), Wiwat Tirapanich, Wiwat Tirapanich, Sopon Jirasiritum, Surasak Leela-Udomlipi, Piyanut Pootracool, and Suthas Horsirimanont
Central vein stenosis in hemodialysis patients can be treated with angioplasty together with stenting, although there is a high incidence of restenosis. This study compared cutting to noncutting balloon angioplasty on the success rate (primary outcome) and the restenosis rate (secondary outcome). The hypothesis was that the low pressure used in the cutting balloon technique would result in less strain on the vessel wall, which would reduce any intimal proliferation and lower the restenosis rate. Successful treatment was defined as a residual stenosis less than 30%, resolution of upper extremity symptoms, and an improvement in elevated venous pressures during dialysis. The cutting balloon technique necessitated a lower inflation time. The between-group success rates were similar (P=0.132) and the restenosis rates were not statistically different (P>0.05). In conclusion, although cutting balloon angioplasty seemed safe, the results did not reach statistical significance compared with noncutting balloon angioplasty.
Shared decisions in vascular medicine
Shared decision making: concept, evidence and development in France
Nora Moumjid (France)
Although shared decision-making is an important aspect in empowering patients in France, it is not as developed as either patient information, which is a regulatory requirement, or therapeutic education. Shared decision-making is a process where the health care professional and the patient exchange information to achieve an agreement regarding a specific decision. Consequently, the exchange of information has to be bilateral and the decision should result from an interactive deliberation. There are several stages in the process: (i) define the situation; (ii) verbalize that there is a decision to make; (iii) present the options; (iv) discuss the potential pros and cons; (v) identify the patient’s preferences; (vi) be sure to have the correct understanding of the patient; (vii) make a decision and be capable of anticipating the next steps. Studies have shown that a practice based on shared decision-making in prevention, primary care, or chronic disease management improves the safety and quality of care, the agreement and communication between health care professionals and patients, and the rights and knowledge of the patients, and it may reduce costs in certain situations. Some of the challenges for the future include: (i) making sure that everyone is talking about the same concept when discussing shared decisionmaking between professionals and patients; (ii) be able to develop multidisciplinary projects for intervention and implementation; (iii) determine how to mobilize health care professionals, decision-makers, and public funders.
The patient’s perspective
Eliane Rosay (France)
Eliane Rosay described her expectations when being treated for a disease. She detailed the problems she had when she developed primary lymphedema during her pregnancy, 30 years ago. She emphasized that she had wanted to be treated as a person with a disease instead of a disease. As such, she said she felt abandoned, and therefore, she did not comply with the recommended treatments. Finally, she discovered the multidisciplinary team in Paris at the Hôpital Cognacq-Jay, where everybody was keen on explaining all available techniques in each context and understanding each patient’s particularities. She concluded by stating that the fundamental aspect of making decisions is that health care professionals should look at the patients as humans and not just as a disease.
Best papers of the ESVM 2016 meeting
Hedgehog signaling in human brain arteriovenous malformations
Roberto Pola and Paulo Tondi (Italy)
Hedgehog proteins are morphogens that play an important role in angiogenesis and vascular development. Recent findings suggest a role for hedgehog signaling in the pathogenesis of brain arteriovenous malformations. This study evaluated the hypothesis that an angiogenic growth with the characteristic features of arteriovenous malformations may be obtained by activating the hedgehog-signaling pathway and investigating the expression levels of the various components of the hedgehog-signaling pathway in humans with arteriovenous malformations. Among the various components of the hedgehog pathway, the hedgehog inhibitory protein was significantly and constantly downregulated in all human brain arteriovenous malformation specimens compared with controls. When pellets containing Sonic hedgehog were implanted into the cornea of ephrinB2-lacZ mice, the resulting angiogenic process was characterized by the growth of both arterial and venous vessels that were interconnected with a complex set of arteriovenous shunts without an interposed capillary bed, as has been seen with arteriovenous malformations in humans. These findings show that the hedgehog inhibitory protein is downregulated consistently and significantly in brain arteriovenous malformations. Moreover, the activation of the hedgehog signaling pathway results in a robust angiogenic process that is characterized by the growth of both arteries and veins, with several arteriovenous shunts, which mimic the angle of abnormal vessels observed in human arteriovenous malformations. Taken together, these data strengthen the hypothesis that the hedgehog pathway might play a role in the pathogenesis of arteriovenous malformations, with potentially important clinical implications.
Vascular remodeling in hypertensive patients with well controlled BP values
Massimo Puato and Giacomo Buso (Italy)
This study evaluated the impact of well-controlled blood pressure levels on structural and functional properties of arteries in hypertensive subjects. The authors studied 80 patients who had either been kept on pharmacological treatment (n=55) or lifestyle modification (n=25) for at least 12 months to maintain their target blood pressure. The mean carotid intima-media thickness and the maximum intima-media thickness were assessed in several carotid artery segments bilaterally using a B-mode ultrasound evaluation. Moreover, endothelial function was evaluated using post occlusion flow mediated dilation of the brachial artery and arterial elastic properties were evaluated by assessing carotid distensibility and carotid compliance. A total of 40 normotensive subjects, who were paired for age and sex, served as controls. In well-controlled hypertensive patients, proatherogenic remodeling was still present in normotensive controls. Structural impairment (intima-media thickness) was mainly dependent upon age, whereas functional impairment (flow-mediated dilation) was related to cholesterol levels. Moreover, carotid elasticity was impaired in hypertensive subjects. Therefore, the “pseudo-normalization” of the blood pressure levels does not seem to be sufficient to eliminate the hypertensive status that contributes to functional and structural impairment.