NEW INSIGHTS IN VASCULAR DISEASE
LECTURES
The management of chronic venous disease of the legs in 2004: challenges and opportunities
P. GLOVICZKI (USA)
The lecture was an update on the treatment of chronic venous disease, based on the experience of the speaker and his colleagues at the Mayo Clinic. Venous disease is widespread in the industrialized world, and it ranges from cosmetic problems to the worst complications of the post-thrombotic syndrome. Ninety percent of venous problems are caused by reflux, and less that 10% is caused by venous obstruction. Even in 2004, high ligation and stripping of the saphenous vein is the most effective treatment and the gold standard for decreasing venous reflux, against which all other methods must be compared. Most of the venous operations performed at the Mayo Clinic are of this kind, 1547 high ligation and stripping, compared with 171 SEPS (subfascial endoscopic perforator surgery) for interruption of perforating veins. Recent data from Dwerryhouse (1999) has shown that performing stripping after ligation decreases the recurrence rate from about 25% to a fourth of this number. Even if the results are quite good, the recurrence rate appears to be anywhere between 6% and 26%, and the operation is an invasive procedure. So new methods have been developed, based on endoscopic surgical procedures that aim to obliterate the saphenous vein using radiofrequency and endovascular laser. Radiofrequency ablation cannot be used in subcutaneous, tortuous, or very large vessels. Results at 4 years appear to be very good, with absence of reflux in 86% of the patients, and no varicose veins in 79%. Randomized clinical trials (EVOLVeS) are on their way, to compare this technique with stripping. Very good results for laser endovascular therapy (EVLT) were reported by Dr Min and his group, with 98% immediate and 93.4% 2-year success, and with no deep vein thrombosis complications. Expansion of this experience has of course given slightly different results, and probably these results, including the appearance of a few cases of deep vein thrombosis, which are more representative of the real world. The possibility of thrombus extension to the femoral vein is a concern with both endovascular techniques. In the author’s experience, heparin prophylaxis, early ambulation, and infiltrating the tissues with tumescence solution appear to be important prerequisites for a successful laser intervention. Recently, EVLT is representing an increasing part of the intervention performed at the Mayo clinic. Power phlebectomy and foam sclerotherapy still need to be validated in this setting. The SEPS procedure has led to rapid healing of the venous ulcers that prompted the operation, but the recurrence rate is still high: 15% at 4 years. Foam sclerotherapy of the perforators still needs to be compared with the SEPS procedure, and to be validated. Occlusive disease of the deep veins can still be treated with traditional options like the Palma crossover graft, or with open surgery, but in most cases the primary option is endovascular, and deep vein stenting has positively changed the approach to venous outflow obstruction. Deep vein reconstruction, both open surgery or endovenous, appears to be limited to a relatively small number of patients, but in the author’s opinion its future is bright.
President: C. ALLEGRA (Italy) Chairpersons: P. L. ANTIGNANI (Italy), B. EKLOF (USA)
The revision of the CEAP classification
B. EKLOF (USA)
The CEAP classification is the internationally accepted classification of chronic venous disease based on Clinical manifestations, Etiologic factors, Anatomy, and Pathophysiologic findings. It is 10 years old, and has been published in at least eight languages. Important contributions have been made at several meetings in the last few years, and in 2004 the results of the work of an ad hoc committee of the American Venous Forum will be published. Some of the problems that will be addressed are a more refined description of the C, differentiating reticular veins from varices at a diameter of 3 mm, the role of the corona phlebectatica, adding to the P a Pn grade, meaning “No identifiable venous pathophysiology.” The date of the examination will be added, and also the level of investigation. The first level is the office visit; the second level is a noninvasive examination, such as Color Doppler and plethysmography, and a third level will be a complex or invasive exploration. The present structure will be maintained, but it will be made more precise, and at the same time there will exist a basic CEAP for clinical use, and a more complete one, intended mainly as a research tool. Many issues remain unresolved, but the CEAP has proved to be a tool that helps us all to talk the same language world wide, and its future will be bright.
Epidemiology of CVI and CEAP
A. JAWIEN (Poland)
There are many epidemiological studies on chronic venous insufficiency, but the lack of a uniform classification has made it impossible to get comparable results. The author presented his study, based on the CEAP classification, and his findings on a population study of more than 40 000 people, taken from patients 18 years and older, studied initially by general practitioners. A subgroup of 351 patients was studied with Duplex, for a total of 702 legs. One of the key messages from this study is that among the CEAP parameters, the disability score is the one that correlates less with the clinical classes (C), but more work must be done.
Prognostic value of the corona phlebectatica and CEAP classification
P. CARPENTIER, M.T. WIDMER (France)
Corona phlebectatica is defined as fan-shaped intradermal telangectases on the medial or lateral aspect of the foot, and although it is part of the C1 (CEAP) class definition, there is controversy on the importance of this finding as a prognostic tool. To assess this problem, the authors used the data of the Basel study, which in 1971 enrolled 4502 workers from the chemical industries of Basel. In 1982 1441 subjects were selected, with a bias towards people with venous problems, and a complete clinical and photographic assessment was kept for each patient, which allowed the authors to reclassify the subjects according to the CEAP classification. There were only nine patients who presented with venous ulceration at the end of the study, but considering the presence of skin trophic changes, the presence of corona phlebectatica was one of the strongest clinical predictors of further occurrence of skin trophic changes. The authors propose including it in a revised CEAP classification, despite comments from others indicating that this finding is widespread, and are questioning its utility in the CEAP classification.
CEAP and instrumental evaluation
C. ALLEGRA (Italy)
Professor Allegra stressed the concept that the CEAP classification is an evaluation criterion that offers an objective and synthetic picture of chronic venous disease (CVD), and not some sort of computerized medical record. Simplicity and usability must be the keynotes of this classification. One of the most useful investigations in most situations appears to be the duplex scanner – color Doppler, with phlebography reserved for the study of congenital disease, and water volumetry used for the objective assessment of edema. Newer techniques, such as nuclear magnetic resonance or computerized tomography, have to prove their work. Older techniques, such as Doppler tensiometry by Bartolo, could find new applications. Clinical findings always have a pivotal role.
Computer venous registry: how to make CEAP more useful in your practice
J. F. UHL (France) A. Cornu-Thenard (France) was unable to attend the meeting, so his place was taken by Dr Uhl, who described and then made a live presentation of the CVR software, used to give a real-time CEAP assessment of venous disease in our patients, following simple instructions on the screen. The program is freely distributed, and available on a CD.
Proposal for the future
J. F. UHL (France)
CEAP has always been seen as a dynamic tool that must be modified, without compromising its stability. It is still being modified, but there is the need for more solid epidemiological data for a better understanding of chronic venous disease. The CEAP will be divided into a simple CEAP for routine clinical practice, and an advanced CEAP, mainly used for research. To the CEAP classification, a Pn will be added to the P part, meaning normal findings, and the date of observation and level of investigation will be added. There is the need to better assess the C2 group, into which most of the patients appear to be classified. An interesting concept is that of the venous imputability score, used to assess which symptoms are attributable to varicose veins, and which are not. A lot of work remains to be done, but the CEAP classification is an extremely useful standard, and it is here to stay.
CEAP: a never-ending “Tower of Babel”
H. PARTSCH (Austria)
The author showed a series of clinical cases where acrodermatitis chronica atrophicans, muscle hernia, Kaposi sarcoma, erysipelas, lymphoma, and other diseases could be easily confused with venous disease. His recommendation is that the CEAP classification system should include a clear differentiation from nonvenous diseases.
President: C. ALLEGRA (Italy) Chairpersons: R. SIMKIN (Argentina), J. ULLOA (Colombia) With the participation of J. H. ULLOA, J. ULLOA (Colombia), I. PIZARRO, F. IBANEZ, C. SALAS, A. CAM, J.A. PARRA, V. BIANCHI (Chile), R. SIMKIN, R. BULLOJ, C. SIMKIN (Argentina), M.E. RENNO DE CASTRO SANTOS (Brazil)
Ulloa reported about new agent for sclerotherapylapidium chloride (LC.) It is more effective and safer in comparison with ethanolamine oleate (EO) and polidocanol. Important advantages of LC were the high degree of adhesion of a venous wall and the long period it remained in a microfoam state. Also, there was a smaller range of complications, such as thrombosis, hyperpigmentation, and hemolysis. Pizzarro presented follow-up results (from 3 months to 3 years) of surgical treatment of 16 limbs (14 patients) with deep venous insufficiency (reflux, obstruction, or combination reflux and obstruction) and venous ulcers. Different operations were performed. There were combinations of Palma and Husni operations, transposition of the superficial femoral vein below the competent valves of the deep femoral vein or internal saphenous vein; and transfer of the axillary vein into superficial femoral vein position. The authors drew the conclusion that individually picked up volume of operation allows correction of chronic deep venous insufficiency and achievement of healing of ulcers in 75% of cases. R. Simkin reported on combination surgical treatment of primary varicose veins. Combination of ambulatory phlebectomy, endovenous laser treatment, and subfascial endoscopic perforator surgery was used. The inversion technique or partial resection were the methods for the removal of the incompetent long saphenous vein. Short saphenous vein incompetence was treated with stripping or endoluminal laser coagulation. The authors concluded that such a surgical technique allows minimization of postoperative complications and achievement of good follow-up results. Renno de Castro Santos noted that recurrent varicose veins occur in 7% to 80% of cases. The author emphasized that it is necessary to differentiate true recurrent varicose and residual veins. True recurrent varicose veins are absent in the early postoperative period, while residual veins can be demonstrated immediately after operation. It is necessary to use various diagnostic tests (clinical examination, handheld Doppler, duplex scanning or phlebography, and quality of life questionnaires) reveal the reasons for recurrent varicose veins.
Chairpersons: J. ULLOA (Colombia), R. SIMKIN (Argentina) With the participation of A. SCUDERI (Brazil), P. KOMLOS (Brazil), H. GUEDES (Brazil)
Scuderi emphasized that badly applied bandages after surgical treatment of varicose veins can cause serious complications. That is why, for the last 20 years, the author has preferred to use a sterile compression stocking which is placed on the leg at the end of the operation. This has allowed him to lower considerably the frequency of edemas and hematomas in the postoperative period, and also to provide the patient with the necessary comfort. Komlos reported his experience with 1780 operations concerning primary varicose veins. He used epidural (85% of cases) or local (15% of cases) anesthesia. The author performs a small vertical incision above the inguinal fold for crossectomy. Long or short saphenous veins were removed by stripping. Small varicose branches were eliminated with crochet hooks and sclerotherapy. The author achieved good long-term results in all cases with a minimum number of minor complications. Guedes reported the summaries of the 1st Latin American Consensus of Lymphedema (March, 21-23, 2003). Thirty-two leading experts from Latin-American countries took part. It was pointed out that lymphedema is characterized by two basic parameters: liquid and protein accumulation in the intercellular space; and internal or external manifestation of the insufficient lymphatic system. It was decided to distinguish between primary lymphedema connected with dysplasia of the lymphatic vessels and secondary to trauma or an infection. It was proposed that history, clinical sympoms (including Stemmer’s sign), results of lymphoscintigraphy, and capillaroscopy should be used for diagnostic of lymphedema. The basis of treatment of lymphedema is compounded by complex physical therapy which includes manual drainage and an intermittent pneumatic compression. Also, it is necessary to use a combination diosmin/hesperidin, 5,6 alfa benzopyrones for oral or topical administration, and sometimes diuretics. Antiparasitic drugs are necessary for elimination of Filaria. Indications for surgical treatment are the following: penoscrotal lymphedema, morbid obesity, and giant forms. Microsurgery can be effective at the early stages of lymphedema. The author concluded that combination and permanent treatment of lymphedema protects against infection complications, fibrosis, and lymphosarcoma.
Chairpersons: N. ALLAF (UK), R. MARTINEZ (Italy)
Tumescent liposuction anesthesia for varicose vein surgery
M. SIMKA, M. PULTORAK (Poland)
Operation for varicose veins can be performed under: – general anesthesia – spinal anesthesia – or local anesthesia. Each of these methods has advantages and disadvantages. General and spinal anesthesia are widely used, mainly in hospitals. They make it easy for the surgeon to operate. However, general anesthesia requires a hospital stay, is expensive, and may be associated with toxic reaction. Spinal anesthesia can be associated with increased intraoperative and postoperative bleeding. Local anesthesia is believed to be the best choice for the majority of patients. The main problems associated with local anesthesia in varicose vein surgery are: the presence of intraoperative pain and the toxic reaction to the anesthetics, which is usually due to overdose. The authors presented the method based on the tumescent liposuction fluid developed by Geoffrey Klein, which seems to be very well tolerated and safe. No toxic reactions were reported, even with a dose of lidocaine up to 50 mg/body kg –which for an average patient is equivalent to 3.5 liters of anesthetic fluid. Components for 1 liter: – physiologic saline (0.9% NaCl) 1000 mL – lidocaine 1000 mg – (0.1% solution) – sodium bicarbonate – 10 m Eq – epinephrine – 1 mg – triamcinolane – 10 mg The authors emphasized that it is very important to warm it up to about 40°C, to avoid stimulation of pain receptors that are very sensitive to cold and to introduce the anesthetic fluid slowly, thus avoiding unpleasant sensations. When stripping of the saphenous vein is planed, it is better to use a more concentrated solution. The advantages of this method are: – the anesthesia is safe – the injection of anesthetic fluid is nearly painless, as it is warm and neutral – lidocaine acts mainly locally – there is minimal bleeding because with the use of epinephrine the blood vessels are contracted. The authors compared 20 patients who were anesthetized with Klein’s solution with those who received classic local anesthesia. It was found that Klein’s anesthesia was associated with less pain, less bleeding, and postoperative hematomas were smaller.
New posterior video-assisted approach to subfascial perforating vein surgery (VASPS)
C. CAMPISI, F. BOCCARDO (Italy)
The subfascial endoscopic ligation of perforating veins allows for accurate treatment of their incompetence. Over the last few years this procedure has been using the medial approach. According to the authors, poor results with lateral subfascial endoscopic perforatory vein surgery seem to be related to misinterpreted perforator anatomy. For this reason the authors proposed a new posterior video-assisted surgical approach. Over a period of 2 – years, video-assisted subfascial perforating vein surgery on both medial and lateral site of the leg in 7 patients were performed. Two 5-to-7 cm incisions, the first one in the middle 1/3 of the posterior aspect of the leg and the second one in the lower 1/3, again on the posterior aspect, were made. Diagnosis was performed by means of phlebography and duplex scanning. Postoperative duplex scans showed the absence of incompetent perforating veins in 5 patients. Despite the small number of patients involved in the examination, video-assisted subfascial perforator vein surgery proved to be a safe and an effective procedure in the treatment of severe chronic venous insufficiency caused by incompetent perforating veins in the calf.
Honorary Chairpersons: M. FÖLDI (Germany) A. LEDUC (Belgium), M. OHKUMA (Japan) Chairpersons: E. AROSIO (Italy), C. CASSAR (UK)
Inflammatory reaction in venous valves induced by venous hypertension is reduced by MPFF
S. TAKASE, L. PASCARELLA, M. E. PUEYO, J. J. BERGAN, G. W. SCHMID-SCHÖNBEIN (USA and France)
In the USA, chronic venous disease (CVD) is a burden for society. CVD is ranked third in the USA by the Vascular Disease Foundation, after lowerlimb arteriopathy and aortic aneurysm. Prevalence of CVD in the USA is 27% in the adult population, while it is 13% in France. Early management of CVD is believed to be the best way to avoid the costs of this disease. Researchers from the Whitaker Institute for Biomedical Engineering of California University in San Diego set up an animal model that mimics venous hypertension in human beings. The objective of their study was, in the first instance, to investigate the mechanism of valve destruction in the saphenous veins. In the second instance, the effect of micronized purified flavonoid fraction (MPFF) on the mechanism of valve destruction was evaluated. Chronic venous hypertension was induced by the creation of an arteriovenous fistula (AVF) in Wistar rats. The subsequent venous hypertension was associated with an inflammatory reaction in the venous valves. Animals were divided into 3 groups: 1 control, 1 treated with MPFF 500 mg/kg/day and 1 treated by MPFF 100 mg/kg/day. After 3 weeks during which animals were submitted to venous hypertension, the morphology of the saphenous valves was examined and the inflammatory markers assessed. The MPFF treatment reduced the shortening of leaflets. In parallel, the reflux flow was inhibited by MPFF in a dependent manner. Also, the number of adherent leukocytes and their migration across the postcapillary venules was reduced by MPFF. These results suggest that MPFF reduces the inflammatory reaction associated with venous hypertension. In CVD, MPFF might protect venous valves from destruction.
SYMPOSIUM IUA/GEL (EUROPEAN LYMPHOLOGY GROUP)
Honorary Chairpersons: M. FÖLDI (Germany), A. LEDUC (Belgium), M. OHKUMA (Japan) Chairpersons: P. BOURGEOIS (Belgium), C. CAMPISI (Italy) The symposium offered an overview of the various methods used, and the main research topics with which doctors from all over the world are involved.
Intermittent compression therapy: to use or not to use? A review of the literature
J. P. BELGRADO (Belgium)
Intermittent compression therapy is the application of force on an edema, to evacuate its components as much as possible. Many methods are used to reach this goal, ranging from mercury baths to pneumatic devices, but the latter are the only ones used on a large scale. Unfortunately, not only are there few wellconducted studies on this topic, but also they vary extremely in all aspects. The machines can be mono-or multichambered; now only the multichambered ones are used, as they give better results, but the number of chambers can vary from 3 to 24, and there are no studies that tell us whether there is any difference between them. The sleeves can be rigid, made of PVC, and tend not to conform to the leg contour, or are made of Hypalon, which is soft and gives better results and comfort for the patients. Most studies rely on the pressure that is shown by the machine manometer, but it is often more than indicated, and can be even higher if measured directly on the skin – even twice the theoretical value. The pressures exerted by manual drainage are usually about 8 millimetres of mercury, while the target pressure can be anywhere from 30 to 80 millimetres. The cycles can vary from 5 to 25 seconds’ inflating time, and 20 to 30 seconds’ deflating time. The sessions can last from 1 to 8 hours, and in some studies intermittent pneumatic compression is used by itself, while sometime it follows manual drainage or compression therapy. Even the outcomes are measured in different ways, and it is almost impossible to compare different studies. Obviously some form of standardization and more extensive studies are needed.
Prevention of secondary arm lymphedema: diagnostic and therapeutic strategies
F. BOCCARDO (Italy)
The authors reported their experience in a small group of selected patients who underwent conservative surgery for breast cancer. If preoperative lymphoscintigraphy showed impaired circulation in the arm to be treated, microsurgery was performed at the time of lymph node dissection, to restore drainage, and the results were good in the few treated patients.
Complete decongestive treatment in lymphedema
E. FÖLDI (Germany)
The author reported on her experience in a 140-bed clinic for lymphatic disorders, where patients are treated in an integrated way with manual drainage, additional massage, compression bandage, skin care, individually fitted compression garments, and so on. Two thirds of the patients have other diseases, such as congestive heart failure, and so a medical checkup is very important, as well as the collaboration of trained and motivated physiotherapists. Patient education, for skin wound prevention, body weight regulation, and increased physical activity is of paramount importance, and increases with patient compliance. Using this approach, the results are good and are maintained for up to 4 years.
Complications of pelvic lymphadenectomy
E. IKER (USA)
The author presented a series of 25 patients with various degrees of lymphatic problems in the legs and groin after different kinds of surgical intervention for cancer. It is important that such symptoms are identified early, and surgeons pay more attention to the preservation of lymphatic pathways when operating on this kind of patients, as is now practised in breast cancer patients.
Rehabilitation protocol in upper-limb lymphedema
O. LEDUC (Belgium)
Even with intensive treatment, sometimes patients retain a volume difference between the affected upper limb and the normal limb. Using MRI the author has shown that in some cases fat accumulation, intermixed with fluid accumulation, is responsible for this durable volume increase.
Management of primary and secondary lymphedema
S. MICHELINI (Italy)
The author showed the results obtained in his lymphedema clinic, using a complex approach to these patients, that includes several specialists, considers psychological aspects, and teaches selftreatment, to maintain a volume reduction of the limb of up to one third after 2 years.
Effectiveness of long-term penicillin in dermatolymphangioadenitis
W. OLSZEWSKI (Poland)
Filarial lymphedema is a widespread disease in the third world, and the disease affects millions of people. In rural India there is widespread use of locally produced penicillin, Penidur, for long periods of time, to avoid the main complication of lymphedema, that is, recurrent episodes of dermatolymphadenitis (DLA). The author studied a group of 40 patients who underwent a treatment with intramuscular injection of 1 200 000 units of Penidur every 3 weeks, for 1 year or more, after one or more episodes of DLA, and compared them with another group of 34 patients who for several reasons were unable to receive the same treatment. In the treated group there were recurrences in 5.6% of the patients, while in the nontreated group recurrences were as high as 76.4%. There were fewer bacteria isolated in the lymph, tissue fluids, and subcutis of the treated group, but more in the lymph nodes. No appreciable change in sensitivity to most antibiotics was found in the treated patients. These data support the use of penicillin for long periods of time in filarial lymphedema to avoid DLA complication.
Prevention of lymphedema. Hazard or fatality?
A. PISSAS (France)
Activity of the Lymphology Centre of the University Hospital of Nancy, Eastern France
G. THIBAUT (France)
Both authors reported their experience in their respective clinics, stressing the importance of prevention, and the role that scars have in disrupting lymphatic flow after surgical interventions.
Genetics of lymphedema – angiodysplasia syndromes: past, present, and future
M. WITTE (USA)
Molecular biology methods can be used to study the numerous (more than 40) familial syndromes that involve lymphedema – angiodysplasia. These syndromes have been known for many years, but only recently gene mutations and chromosomal anomalies have been linked to these diseases. Mutant mice and other sophisticated techniques were used to identify such anomalies, but there is the possibility that in the future, gene therapy and other novel techniques could control such conditions.
Lymphorrhea
M. OHKUMA (Japan)
Lymphorrhea is a complication that affects about 3% of patients with lymphedema, involves the exudate of lymph, and can be divided into oozing and vesicles. The author obtained good results in these cases using a machine that involves magnetic field, vibration, and compression.
LECTURES
Follow-up and natural history after venous thrombosis: the interaction between reflux, lysis, and recanalization
A. MARKEL (Israel)
Deep venous thrombosis (DVT) is a very important medical problem. Pulmonary embolism and postthrombotic syndrome are common complications of DVT. Clinical pulmonary embolism occurs in 26% to 67% of the cases with a mortality rate of 11% to 23%. Anticoagulant therapy begun on time reduces the hazard of pulmonary embolism up to 5% and mortality rate decrease less than 1%. A frequent outcome after DVT is recanalization with restoration of the venous lumen. The basic mechanisms producing recanalization are clot retraction and thrombolysis. Rapid spontaneous or stimulated thrombolysis provides a better prognosis for preservation of valvular function with decreased incidence of reflux. Clot retraction and organization is the basic mechanism of valve cusp injury. The incidence of reflux increases in the months following DVT through the first year. Reflux occurs in about two thirds of limbs after an episode of DVT. Chronic venous insufficiency (CVI) can develop irrespective of localization of the reflux in the deep or superficial venous system. The high risk of CVI increases in patients with reflux in several venous segments. Ulcers occur more frequently with distal thrombosis. Superficial reflux contributes to the development of the postthrombotic syndrome. A combination of deep and superficial reflux, especially in distal veins, plays a critical role in the pathogenesis of the postthrombotic syndrome and ulceration.
Chairpersons: J. FLETCHER (Australia), E. MARCHITELLI (Italy)
Venous thromboembolism and spinal surgery
J. FLETCHER (Australia)
Combined DVT prevention in acute spinal cord-injured patients
A. PIERI, S. AITO, F. MARCELLI, M. D’ANDREA, M. SANTINI, M. GATTI, A. CARNEMOLLA (Italy)
There are a few well-known risk factors for developing deep vein thrombosis following spinal surgery: – duration of operative procedure – prolonged postoperative recumbence – vessel manipulation during anterior surgical approaches – compression of the femoral venous system depending on positioning of patients. The effectiveness of venous thromboembolism (VTE) prophylaxis in orthopedic surgery is well documented. A. Pieri et al demonstrated that combined primary DVT prevention (mechanical plus pharmacological) seems to be a valuable method in acute spinal cord injury patients. Due to the possibility of development of spinal hematoma, surgeons are reluctant to use heparin as a VTE prophylaxis. To assess the incidence of VTE in patients undergoing spinal surgery 170 consecutive patients between January 2000 and December 2003 were examined. Bilateral lower-extremity venous duplex scan was performed preoperatively, within 1 week and 4 to 6 weeks after operation. Mechanical prophylaxis (graduated compression stockings, intermittent pneumatic compression, and early postoperative ambulation) were used in all patients. Heparin was used in 60.5% of patients: – commenced preoperatively in 16.3% – commenced postoperatively in 44.2% The author’s findings showed that following elective spinal surgery where mechanical prophylaxis was applied with selective use of heparin, the incidence of DVT was relatively low at 3.6 %; 1.2% occurred after hospital discharge. There was a surprisingly high incidence of preoperative abnormality in 36.3% of patients (33.3 % superficial thrombophlebitis, 3% developed DVT). These abnormalities may possibly reflect patient immobility prior to spinal surgery. There is a need for caution when interpreting findings of DVT; these should be interpreted with great caution if only postoperative scanning is utilized.
Deep venous thrombosis: polymorphonuclear leukocyte integrin profile
G. CAIMI, M.G. TOZZI, C. CAROLLO, B. CANINO, M. MONTANA, F. FERRARA, R. Lo PRESTI (Italy)
During deep venous thrombosis (DVT) thrombogenesis is accompanied by an inflammatory response, and both processes require an interaction between circulating cells and endothelium. The initial reversible interaction between leukocytes and endothelium is mediated by selectins, while firm adhesion of polymorphonuclear leukocytes (PMN) and their subsequent transendothelial migration need the expression of B2 integrins on PMNs. B2 integrins interact with their corresponding endothelial counterligands, especially intercellular adhesion molecule-1 (ICAM-1) and allow PMN to attach and to go across the endothelium. The expression of B2 integrins increases after activation, stimulated during thrombogenesis by thrombin and local production of proinflammatory cytokines. Up to now there have only been a few data regarding PMN integrin pattern in chronic venous disease and no data in DVT. The aim of the study was to examine, in subjects with acute leg DVT, the PMN B2 integrin pattern (CD11a, CD11b, CD11c, CD18). 19 patients with unilateral lowerlimb thrombosis were studied. The decrease in the basal expression of CD11b, which has a key role in the interaction between PMNs and endothelium, has been also observed as a result of short-term venous hypertension in subjects with chronic venous disease. The increase in the basal expression of CD11c may be related to the spontaneous PMN activation, the latter is confirmed, in these subjects, by the increase in PMN cytosolic Ca 2+ content. In DVT subjects after PMN activation the authors observed an increase in all the integrins with the exception of CD11. These data can add some new information to an aspect of DVT which may have therapeutic implications. Up to now the anti-integrin treatment has been investigated in arterial vascular diseases with controversial results. Considering the availability of well-tolerated molecules, DVT may be a new target, especially with the aim of preventing the post-thrombotic syndrome.
Superficial thrombophlebitis as a clinical sign underlying a systemic condition
E. MARCHITELLI, R. PEPE, R. GLORIA, D. MONETTI (Italy)
Superficial thrombophlebitis is a common condition often observed in patients with varicose veins. It is generally considered as a benign, self-limiting disease, despite numerous reports of prolongation of clot into the deep vein system and the development of pulmonary embolism. The authors of the paper consider that in the presence of idiopathic superficial thormbophlebitis, an extended diagnostic investigation should be performed. In 16 patients with varicose veins and in 18 with normal veins superficial thrombophlebitis was observed. In 18 patients without varices, apparently idiopathic, positivity for immunological diseases (6 patients), tumors (5 patients), as well as abnormal coagulation profile (4 patients) were found. The authors concluded that the real incidence of STV and its thromboembolic complications is still undefined. Duplex Doppler scanning must be performed in all cases, in order to assess the real extension of thrombus in the superficial and deep venous systems. The underlying conditions must be investigated in cases of idiopathic and/or recurrent superficial thrombophlebitis with or without varicose veins.
Ambulatory treatment of DVT of lower limbs
E. DI NARDO, M.R. VILLANI, N. FEDERICI (Italy)
Deep vein thrombosis is the third most common cardiovascular disorder in the western countries. Twenty to 40% of proximal DVTs are complicated by pulmonary embolism. The standard treatment of DVT includes: hospital admission, bedrest, infusion of unfractioned heparin with subsequent compression and walking. The authors proved that ambulatory treatment is effective and is not associated with an increased danger of pulmonary embolism. Forty – four patients suffering from DVT in one or more segments of deep leg veins were examined. Proximal extension of thrombus: – 9 patients-femoro-iliac segment – 21 patients-popliteal femoral segment – 14 patients-below popliteal segment All patients received LMWH for 1 month and then 6 months’ oral anticoagulation therapy with compression stockings. A follow-up was performed with duplex at 1.3, and 6 months’ and CT-scanner at 6 months. No patients had pulmonary embolism episodes. Three patients required hospitalization for caval filter implantation. Thirty patients with complete followup had no other symptoms or complications. In the discussion it was underlined that patients with DVT and suspicion of pulmonary embolism need to be hospitalized.
Residual vein thrombosis establishes the optimal duration of oral anticoagulants for the treatment of DVT
S. SIRAGUSA (Italy)
The optimal duration of anticoagulant therapy (OAT) after a first episode of deep-vein thrombosis (DVT) is still uncertain. Agnelli et al reported that long-term anticoagulation therapy is effective in preventing recurrences, but its benefit is lost after its discontinuation. It would be important to identify the individual risk for recurrences for establishing the appropriate therapy. Residual venous thrombosis (RVT), defined as clot persistence over time detected by venous ultrasonography, has been shown to be an independent risk factor for recurrent VTE. RVT is indicative for an underlying hypercoagulable state since recurrences may occur in the controlateral leg as well. This conclusion applies to patients with both idiopathic and provoked DVT. The advantage of adjusting the duration of oral anticoagulant therapy according to the presence or absence of residual vein thrombosis is still uncertain. The authors performed a randomized controlled trial for evaluating whether the presence/ absence of RVT can help establish the optimal duration of OAT in consecutive patients with a first episode of idiopathic or provoked DVT. Inclusion criteria were the presence of a first episode of proximal DVT (idiopathic or provoked) of the lower limbs, detected by compression ultrasonography. Death and bleeding were the criteria for assessing safety outcomes. Major bleeding was a criterion if clinical, overt, and associated with either a decrease in the hemoglobin level of at least 2 g/L or the need for the transfusion (>2 units) retroperitoneal, or intracranial. Minor bleeding in other circumstances was included. The authors performed an interim analysis on 261 patients who completed a 2-year follow-up. 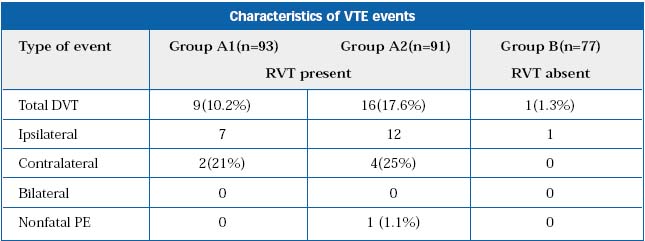 In patients with persistent RVT, 3 months of OAT was associated with a high risk of recurrences (17%). However, the advantage of prolonging OAT is unclear since 1 year of anticoagulation simply delayed the risk of recurrent VTE. In patients without RVT, OAT can be safely withheld after 3 months because of the low risk of recurrence (<2%). The low rate of events remains for up to 21 months and applies to patients with idiopathic or provoked DVT. This study, according to the authors, has a clinical impact: – identifies RVT as a marker for assessing patient’s risk of recurrent VTE – can be applied in patients with either idiopathic or provoked DVT – in idiopathic DVT, absence of RVT allows withholding of OAT (after 3 months) in almost 30% of patients – in provoked DVT, presence of RVT identifies high risk patients who may need prolonged OAT.
In patients with persistent RVT, 3 months of OAT was associated with a high risk of recurrences (17%). However, the advantage of prolonging OAT is unclear since 1 year of anticoagulation simply delayed the risk of recurrent VTE. In patients without RVT, OAT can be safely withheld after 3 months because of the low risk of recurrence (<2%). The low rate of events remains for up to 21 months and applies to patients with idiopathic or provoked DVT. This study, according to the authors, has a clinical impact: – identifies RVT as a marker for assessing patient’s risk of recurrent VTE – can be applied in patients with either idiopathic or provoked DVT – in idiopathic DVT, absence of RVT allows withholding of OAT (after 3 months) in almost 30% of patients – in provoked DVT, presence of RVT identifies high risk patients who may need prolonged OAT.
SYMPOSIUM IUA/SIDV (ITALIAN SOCIETY FOR VASCULAR INVESTIGATION)
Chairpersons: P. L. ANTIGNANI, S. NOVO (Italy)
Cardiac causes of systemic embolism, including aortic arch embolism
D. L. CLEMENT (Belgium)
At least 75% of emboli come from the heart, and atrial fibrillation is the cause in 75% of the cases. The risk of stroke in AF is 3% to 8% per year. Therapy with 325 mg of aspirin in the absence of any risk factors and anticoagulation therapy for all other cases is mandatory. Most of these heart emboli are macroemboli, while many microemboli arise from the aortic arch, and can be dislodged by manipulation following angiography, stenting, or surgery. Some cases are spontaneous, or follow aggressive medical therapy. Transoesophageal echocardiography can help assess this disease and show plaques that can be more than 4 mm thick, but most of these patients are old, with disseminated atherosclerotic disease and fragile, making them difficult to treat. Statins can have a role in plaque stabilization in these patients.
Carotid ulcers as a cause for embolism
C. LIAPIS (Greece)
Of all strokes, 25% can be attributed to carotid plaques. The unstable plaque is the one where the fibrous cap is thin and inflammation is more common. The disruption of the fibrous cap can lead to symptoms. Data from the NASCET and ECST studies indicate that ulcerated plaques double the risk of stroke, and that the irregular plaque is a predictor of adverse effects. Most of these diagnoses are made from angiograms, but an ultrasound assessment would of course be preferable. Randomized studies are on their way, but up to now it seems that echolucent plaques, the ones that look darker and are difficult to distinguish from blood, are the most dangerous ones.
Microembolic events during carotid surgery or endovascular treatment
B. GOSSETTI, O. MARTINELLI, R. STUMPO, F. FACCENA, R. GABRIELLI, M. MARINO, L. IRACE, F. BENEDETTI-VALENTINI (Italy)
The author reported his experience with transcranial Doppler (TCD) monitoring in almost 1000 patients undergoing carotid endoarterectomy, and 45 patients who underwent PTA of the carotid arteries. While microembolic signals are quite common during carotid endoarterectomy, most of them are gaseous in nature, and appear as a shower of bubbles on TCD monitoring. Particulate emboli are much rarer, and in more than 1000 procedures, the clinical complications were 7 strokes, 7 TIAs, and 3 ocular deficits. Most particulate emboli appeared during carotid dissection. TCD showed no emboli in 1 hour of preintervention monitoring, but during PTA emboli were present in all patients without cerebral protection, and were distributed in all phases of the procedure. There was one TIA during angiography, and the use of a protective device, Epifilter, reduced the number of emboli.
Blue toe syndrome
P. POREDOS (Slovenia)
The blue toe syndrome is a localized necrosis of a toe, caused by occlusion of digital arteries by cholesterol crystals and other thrombotic material, in patients that often have palpable pedal pulses. In 97.5% of the cases, the source is widespread atherosclerosis in the aortoiliac and femoral system, often in combination, it is only 2% from aneurysms. The patients are usually elderly, but the ankle brachial index is abnormal in only 37% of the patients, even if the toe pressure is almost always decreased. Different clinical presentations are livedo reticularis, and “trash foot”, where there is major foot damage, while the most dangerous form is the involvement of internal organs, and if the kidneys are affected, mortality can be as high as 70%. The presence of pedal pulses must not lead us astray, and this situation must not be confused with acro syndromes or trauma. Therapy can be difficult in these fragile patients, and the prognosis is usually poor.
Degree of anticoagulation and microembolic signals in patients with prosthetic valves
D. RIGHI (Italy) The author reported on a small series of 47 patients treated with a mechanical prosthetic valve, where the highest number of embolic signals were present in inadequately anticoagulated subjects, supporting the idea that microembolic signals in prosthetic valve patients could be more clinically relevant than previously thought.
Microembolic events during peripheral catheterization and surgery
J. FERNANDES E FERNANDES (Portugal) The final speaker summarized the data that emerged from the session, and stressed the point that in this kind of condition “prevention is the Holy Grail,” our main objective.
LECTURES
Conservative treatment in patients with PAOD: what is evidence-based?
H. RIEGER (Germany)
The high prevalence and incidence of intermittent claudication have a high medical and socioeconomical importance. The author reviews the nonsurgical treatment of this pathology and evaluates evidence-based medicine in the treatment of intermittent claudication with supervised exercise, drugs, and interventional therapy. The evaluation of the results was done in three fields: – walking distance improvement – quality of life – cardiac and neurological evolution related to intermittent claudication The evaluation-based medicine, through several meta-analyses, has demonstrated the efficacy of supervised training exercise in improving walking distance (evidence-based medicine 1a). In relation to drugs, only naftidrofuryl, the prostanoids, and cilostazol have demonstrated efficacy in intermittent claudication (evidence-based medicine 1a) but their use is only allowed in a few countries. Naftidrofuryl is accepted almost all countries, cilostazol is only accepted in the USA, UK, Japan and Ireland, and PGE1 is not accepted for to treat intermittent claudication in the majority of countries. Finally, the author recommends the use of endovascular therapy in the iliac and femoropopliteal sector for patients with intermittent claudication. But this recommendation must be revised. Endovascular treatment, based on TASC recommendations, is a good treatment in moderated iliac like type A and B lesions. Probably the most severe lesions, TASC type C and D, could be treated effectively in the future with the development of more suitable balloons and stents. In the femoropopliteal sector endovascular therapy remains controversial. Probably in patients with type A lesions who have controlled risk factors and have not improved after supervised exercise training, endovascular therapy could be indicated. In cases of type B, C, and D lesions there are not clear results and there is not enough evidence to recommend endovascular treatment. There is a lack of evidence regarding long-term results in the treatment of femoropopliteal lesions with endovascular therapy. Several prospective randomized trials have demonstrated improvement of walking distance after 1 year’s follow-up, but not after 2-year follow-up with chronic femoropopliteal lesions which had been treated with angioplasty compared with walking exercise alone. Several meta-analyses, performed in recent years, have demonstrated that endovascular therapy has a definitive role in the femoropopliteal segment, but the exact indication must be defined, since then we must evaluate every case individually before recommending the general use of endovascular therapy in the femoropopliteal sector in patients with intermittent claudication.
Chairpersons: L. NORGREN (Sweden), S. NOVO (Italy)
As Prof Dormandy explained, the TASC document is a consensus which was published in 2000 with the aim of improving care of individual patients suffering from peripheral arterial disease (PAD). It was created by a working group where twelve international associations were represented, including vascular medicine, vascular surgery, and radiology. Methodologically they discussed and included existing acknowledged guidelines and tried to reach a consensus in an evidencebased medicine format. The potential health benefits, risks, and costs incurred from the recommendations were assessed. At the present time, in 2004, there is a need of updated data and possible extension of, or changes to, the original issue. This has been noted by the TASC representatives and they are working on The Essential TASC. Prof Belch pointed out the major achievement of the TASC document, which has been used by trainees as a textbook and has permitted a raised profile of PAD, taking into account the CAD risk of this population and the main importance of claudication symptoms. The different areas where TASC needed to be updated were risk factors, treatment of symptoms, perioperative care, and recommendations. Apart from the general risk factors we generally modify, TASC should consider a more aggressive treatment for hypercholesterolemia and inflammation markers such as fibrinogen. When considering treatment of symptoms, naftidrofuryl and cilostazol should be included for treatment of pain in the legs, and pentoxifiline should be reevaluated because more recent studies are challenging its believed efficacy. Besides, new drugs must be taken into account in the new TASC consensus such as statins, recombinant growth factors, and carnitine. Prof Belch recommended an inclusion of quality of life terms in the new consensus. Perioperative care of this group of patients must be completed with CAD assessment, DVT prophylaxis in all patients, and â- blockers as disoprolol in order to improve surgical outcome. Finally she pointed out the need of avoiding conflicts with other pre-existing guidelines from the different societies using evidence-based medicine form when writing the new consensus. Prof Norgren explained The Essential TASC project. He differentiated two possibilities: rewriting or publishing an addendum. The plan is to produce an abbreviated document (no more than 100 pages), easily available to general practitioners and primary health care individuals, disseminated through National Societies and interesting to countries outside Europe and North America. In summary, the contents will be: epidemiology and risk factors, management of risk factors and coexisting diseases (including CoCaLis project), intermittent claudication, critical limb ischemia, acute limb ischemia, and a technical section on open and endovascular procedures. Finally, Prof Clement presented the CoCaLis project as a clinical approach to the management of the patient with limb ischemia who presents with coronary, carotid, or renal disease. This is a document published in International Angiology in 2000 and updated in 2003, presented as different algorithms showing how to deal with the different situations the PAD patient could encounter.
TransAtlantic interSociety Consensus (TASC): what’s new?
D. L. CLEMENT (Belgium)
The Transatlantic Consensus document aims to set up guidelines that can be used by vascular physicians and surgeons on both sites of the Atlantic. In the present paper, the document published in 2000 will largely be used as a baseline. After proper diagnosis of the disorder, treatment should be focused on controlling the total risk carried by the disease. Intermittent claudication is indeed a major risk factor for developing coronary and carotid artery disease. Checking out risk factors and controlling them is therefore essential in this condition. In this respect the role of antiplatelet drugs such as aspirin or clopidogrel will be highlighted. Stopping nicotine and performing regular exercises, preferably in a supervised class, are very essential approaches to the symptoms – according to recommendations 28 and 29 of the TASC. The new problem is what to prescribe first: low doses of aspirin or clopidogrel? Results of the CAPRIE study suggest that for uncomplicated PAD and high-risk patients, clopidogrel is better than aspirin and should be prescribed first. Many drugs have been developed in the past. Due to recommendation 30 of TASC pentoxifylline, buflomedil, naftidrofuryl, and more recently cilostazol have been shown to objectively improve walking distance, but the improvement for most of them is rather small. Recent studies have also shown that naftidrofuryl is also capable of significantly improving quality of life – NIQOL European Study Program. The role of other drugs such us statins and ACE inhibitors has not been defined. The ASCOT study using atrovastatin has shown a reduction in cardiovascular events from 22% to 14% for statins. Further studies are needed.
Clinical approach in the second and third stages of peripheral obstructive arterial disease
R. MARTINI G. M. ANDREOZZI (Italy)
Fontaine’s second and third stages represent two completely different levels of peripherial arterial disease. The second stage should be assessed keeping in mind that patients are at greater risk of dying from the complications of the atherosclerosis. Claudication needs treatment planned to modify factors responsible for the progression of atherosclerosis and development of atherothrombotic complications such as smoking, diabetes, obesity, hyperlipidemia, hypertension, and raised homocysteine. Long-term and low-dose aspirin and regular supervised walking exercise are likely to be beneficial for legs and general disease. Drugs such as pentoxifylline, naftidrofuryl, or cilostazol improve claudication. Propionyl-l-carnitine has been shown to improve claudication, also improving ischemic muscle metabolism. Ankle brachial pressure index, and a walking test, as well as screening for carotid artery disease or cardiovascular disease should be performed. Diabetic elderly patients walking rarely may not have typical claudication – in these patients a microcirculatory test such as toe pressure or TcpO2 should be performed to predict the onset of chronic limb ischemia. The Second “b” of Fontaine or the severe caludication stage of Rutherford shows a microcirculatory pattern more similar to chronic limb ischemia than to claudication. So in this case clinical decisions about the type of treatment should be based on imaging and/or microcirculatory tests as well patients’ lifestyle on one hand and on estimation of the risk of treatment and predictable period of improvement on the other. The third stage of Fontaine, or rest pain stage, is the onset of chronic limb ischemia. So patients should be assessed keeping in mind that chronic limb ischemia has a poor prognosis for patient limb survival. It is well known that about 60% of patients with PAOD have carotid artery disease or cardiovascular disease, and 40% of patients with cardiovascular disease present with PAOD symptoms. Presentation of leg ulceration at this stage is a less predictable factor for leg amputation than local low blood pressure. So imaging of the arterial tree to rapidly perform revascularization if possible is needed.
SYMPOSIUM IUA/TASC (TRANS ATLANTIC INTERSOCIETY CONSENSUS ON MANAGEMENT OF PERIPHERAL OBSTRUCTIVE ARTERIAL DISEASE)
Chairpersons: L. NORGREN (Sweden), S. NOVO (Italy)
As Prof Dormandy explained, the TASC document is a consensus which was published in 2000 with the aim of improving care of individual patients suffering from peripheral arterial disease (PAD). It was created by a working group where twelve international associations were represented, including vascular medicine, vascular surgery, and radiology. Methodologically they discussed and included existing acknowledged guidelines and tried to reach a consensus in an evidencebased medicine format. The potential health benefits, risks, and costs incurred from the recommendations were assessed. At the present time, in 2004, there is a need of updated data and possible extension of, or changes to, the original issue. This has been noted by the TASC representatives and they are working on The Essential TASC. Prof Belch pointed out the major achievement of the TASC document, which has been used by trainees as a textbook and has permitted a raised profile of PAD, taking into account the CAD risk of this population and the main importance of claudication symptoms. The different areas where TASC needed to be updated were risk factors, treatment of symptoms, perioperative care, and recommendations. Apart from the general risk factors we generally modify, TASC should consider a more aggressive treatment for hypercholesterolemia and inflammation markers such as fibrinogen. When considering treatment of symptoms, naftidrofuryl and cilostazol should be included for treatment of pain in the legs, and pentoxifiline should be reevaluated because more recent studies are challenging its believed efficacy. Besides, new drugs must be taken into account in the new TASC consensus such as statins, recombinant growth factors, and carnitine. Prof Belch recommended an inclusion of quality of life terms in the new consensus. Perioperative care of this group of patients must be completed with CAD assessment, DVT prophylaxis in all patients, and â- blockers as disoprolol in order to improve surgical outcome. Finally she pointed out the need of avoiding conflicts with other pre-existing guidelines from the different societies using evidence-based medicine form when writing the new consensus. Prof Norgren explained The Essential TASC project. He differentiated two possibilities: rewriting or publishing an addendum. The plan is to produce an abbreviated document (no more than 100 pages), easily available to general practitioners and primary health care individuals, disseminated through National Societies and interesting to countries outside Europe and North America. In summary, the contents will be: epidemiology and risk factors, management of risk factors and coexisting diseases (including CoCaLis project), intermittent claudication, critical limb ischemia, acute limb ischemia, and a technical section on open and endovascular procedures. Finally, Prof Clement presented the CoCaLis project as a clinical approach to the management of the patient with limb ischemia who presents with coronary, carotid, or renal disease. This is a document published in International Angiology in 2000 and updated in 2003, presented as different algorithms showing how to deal with the different situations the PAD patient could encounter.
TransAtlantic interSociety Consensus (TASC): what’s new?
D. L. CLEMENT (Belgium)
The Transatlantic Consensus document aims to set up guidelines that can be used by vascular physicians and surgeons on both sites of the Atlantic. In the present paper, the document published in 2000 will largely be used as a baseline. After proper diagnosis of the disorder, treatment should be focused on controlling the total risk carried by the disease. Intermittent claudication is indeed a major risk factor for developing coronary and carotid artery disease. Checking out risk factors and controlling them is therefore essential in this condition. In this respect the role of antiplatelet drugs such as aspirin or clopidogrel will be highlighted. Stopping nicotine and performing regular exercises, preferably in a supervised class, are very essential approaches to the symptoms – according to recommendations 28 and 29 of the TASC. The new problem is what to prescribe first: low doses of aspirin or clopidogrel? Results of the CAPRIE study suggest that for uncomplicated PAD and high-risk patients, clopidogrel is better than aspirin and should be prescribed first. Many drugs have been developed in the past. Due to recommendation 30 of TASC pentoxifylline, buflomedil, naftidrofuryl, and more recently cilostazol have been shown to objectively improve walking distance, but the improvement for most of them is rather small. Recent studies have also shown that naftidrofuryl is also capable of significantly improving quality of life – NIQOL European Study Program. The role of other drugs such us statins and ACE inhibitors has not been defined. The ASCOT study using atrovastatin has shown a reduction in cardiovascular events from 22% to 14% for statins. Further studies are needed.
Clinical approach in the second and third stages of peripheral obstructive arterial disease
R. MARTINI G. M. ANDREOZZI (Italy)
Fontaine’s second and third stages represent two completely different levels of peripherial arterial disease. The second stage should be assessed keeping in mind that patients are at greater risk of dying from the complications of the atherosclerosis. Claudication needs treatment planned to modify factors responsible for the progression of atherosclerosis and development of atherothrombotic complications such as smoking, diabetes, obesity, hyperlipidemia, hypertension, and raised homocysteine. Long-term and low-dose aspirin and regular supervised walking exercise are likely to be beneficial for legs and general disease. Drugs such as pentoxifylline, naftidrofuryl, or cilostazol improve claudication. Propionyl-l-carnitine has been shown to improve claudication, also improving ischemic muscle metabolism. Ankle brachial pressure index, and a walking test, as well as screening for carotid artery disease or cardiovascular disease should be performed. Diabetic elderly patients walking rarely may not have typical claudication – in these patients a microcirculatory test such as toe pressure or TcpO2 should be performed to predict the onset of chronic limb ischemia. The Second “b” of Fontaine or the severe caludication stage of Rutherford shows a microcirculatory pattern more similar to chronic limb ischemia than to claudication. So in this case clinical decisions about the type of treatment should be based on imaging and/or microcirculatory tests as well patients’ lifestyle on one hand and on estimation of the risk of treatment and predictable period of improvement on the other. The third stage of Fontaine, or rest pain stage, is the onset of chronic limb ischemia. So patients should be assessed keeping in mind that chronic limb ischemia has a poor prognosis for patient limb survival. It is well known that about 60% of patients with PAOD have carotid artery disease or cardiovascular disease, and 40% of patients with cardiovascular disease present with PAOD symptoms. Presentation of leg ulceration at this stage is a less predictable factor for leg amputation than local low blood pressure. So imaging of the arterial tree to rapidly perform revascularization if possible is needed.
SYMPOSIUM IUS/SIAPAV (ITALIAN SOCIETY OF ANGIOLOGY AND VASCULAR MEDICINE)
Chairpersons: C. ALLEGRA, M. DI SALVO (Italy)
Epidemiology of PAOD and risk factors
E. HUSSEIN (Egypt)
Peripheral arterial occlusive disease (POAD) is caused in the vast majority of patients by atherosclerosis. The prevalence may vary in different parts of the world. However, outcomes of large studies such as the Framingham and Basle studies indicate an incidence of 1% below the age of 50 years, which rises sharply to around 5% above that age with a much higher male preponderance over females. There are a great number of factors which can increase atherosclerotic prevalence. All of these can be divided into two groups – genetic and metabolic. Genetic factors such as gene polymorphism or congenital hyperlipidemia can improve atherosclerotic changes without any symptoms and signs of disease, even at a young age. Metabolic factors are divided into two groups: – the most important are: arterial hypertension, hypercholesterolemia, diabetes mellitus, and obesity, and the second factors related to lifestyle such as stress and lack of exercise. Each of the risk factors has an independent influence on plaque formation contributing to proliferation, apoptosis, and thrombotic changes inside the plaque and on its surface. Thus, plaque structure varies due to different intensity of influence of specific factors on one hand, and of apoptosis, proliferation, calcification, and inflammatory changes on the other. In addition to the factors which influence plaque progression and internal structure there are a great number of other so-called aggravating risk factors such as hyperviscosity syndrome, polycythemia, leukemia, thrombophilia, lupus erythematosus, anticoagulants, dysfibrinogenemia and arteritis. These are related to thrombotic complications in the macroand micro circulation. The main presentation of atherosclerotic changes is claudication, and progress to critical limb ischemia in only in the minority of these, especially in diabetic patients. Complicated plaque with thrombosis is an endstage PAD related to rest pain, ulcers, and gangrene.
Chairperson: J. J. BELCH (UK)
Introduction: a call to action
J. J. BELCH (UK)
Peripheral arterial disease is a distinct atherotrombotic syndrome that is associated with an elevated risk of cardiovascular and cerebrovascular events. The severity and high prevalence of this disease is underestimated, and multilevel pathologies (coronary, and extracranial vessels, upper-and lower-this limb arteries) are underdiagnosed and this results in undertreatment. In 2003, the Prevention of Atherotrombotic Disease Network, an international, multidisciplinary group, published a “Call-To-Action” paper with the goal of increasing awareness, detection, and treatment of PAD. The key action points were:
• increase awareness of PAD and its consequences
• improve the identification of patients with symptomatic PAD
• initiate screening protocols to increase early detection rates in patients at high risk for PAD
• improve treatment rates among patients diagnosed with symptomatic PAD.
Challenging underdiagnosis and undertreatment in PAD: what must we do?
G. AGNELLI (Italy)
Peripheral arterial disease is a major health risk worldwide. The prevalence is high, the risk of myocardial infarction is up to four times higher, and the risk of stroke two to three times higher than in the general population. The relative 5-year mortality for PAD patients is 44%, while over 10 years, 55% of PAD patients die of coronary artery disease and a further 10% of cerebrovascular disease. Underdiagnosis of PAD is a significant problem, since 41% are symptomatic (33% typical claudication, >50% leg pain on exercise, <5% to 10% critical leg ischemia) and 59% asymptomatic. Diagnosis of PAD is of high clinical importance since only 25% of PAD patients are undergoing effective treatment. The PATHOS project studied the frequency of PAD in 1772 patients (screening ABI) admitted to hospital for myocardial infarction, angina pectoris, stroke, or TIA. The study revealed that 30% of these patients had concomitant PAD.
The objectives of therapy for PAD patients are:
• prevent death and disability
• increase quality of life and walking distance
• save limbs.
Preventing atherotrombotic events with clopidogrel: what we know
W. HIATT (USA)
Atherothrombosis represents the unifying pathophysiology of a broad range of cardiovascular diseases. The Antithrombotic Trialists Collaboration meta-analysis provides ongoing recommendations for the use of low-dose aspirin (ASA) in the secondary prevention of cardiovascular events. However, there are additional medications available to optimize treatment for specific groups within the overall cardiovascular population. Clopidogrel is one of these medications that has been studied in four completed trials.
• CAPRIE: 19185 patients. The study demonstrated that in patients with PAD, clopidogrel was superior to aspirin, providing an overall 24% risk reduction for preventing subsequent cardiovascular events.
• CURE (PCI-CURE): patients with an acute coronary syndrome with unstable angina received a double-blind treatment with aspirin and placebo or with aspirin and clopidogrel. There was a relative risk reduction of 31% provided by the aspirin-clopidogrel combination. A higher bleeding risk was noticed and required a lowering of the aspirin dose.
• CREDO: PCI patients were treated for 3 to 24 hours before intervention with aspirin + placebo or clopidogrel + aspirin. The combination of clopidogrel-aspirin was superior in preventing cardiovascular events.
• MATCH: aspirin did not show additional clinical value in high risk cerebrovascular patients when added to clopidogrel (there was a non-significant relative risk reduction of 6.4%).
New horizons in the management of atherothrombosis: where are we heading?
I. BAUMGARTNER (Switzerland)
Atherotrombosis poses a significant public health risk and is responsible for over 28% of deaths worldwide. Publication of results from clinical trials (CAPRIE, CURE, PCI-CURE, CREDO) confirms the potential role of clopidogrel in reducing cardiovascular events. Ongoing clinical trials help to advance our understanding of atherothrombosis and help to develop future treatment strategies.
• CHARISMA (Clopidogrel for High Atherothrombotic Risk and Ischaemic Stabilisation, Management and Avoidance): a large, phase III, multicenter, randomized, parallel-group, doubleblind trial of clopidogrel versus placebo on top of background therapy including low-dose ASA in patients at high risk of atherothrombotic events.
• CAMPER (Clopidogrel and Aspirin in the Management of Peripheral Endovascular Revascularization): evaluates whether clopidogrel versus placebo, on top of standard therapy including ASA, will lead to an increase in the combined rate of primary patency or survival in subjects following PTA +/- stenting.
• CASPAR (Clopidogrel and ASA in Bypass Surgery for Peripheral ARterial disease): doubleblind, randomized study of clopidogrel versus placebo, on a background of ASA in patients receiving a unilateral below-knee bypass graft.
Chairpersons: W. HIATT (USA), S. NOVO (Italy) LECTURE
Endothelial dysfunction and atherosclerosis: clinical relevance
P. POREDOS (Slovenia)
Healthy endothelium plays a central role in cardiovascular control. Therefore endothelial cell dysfunction (ED) may have a particularly significant role in the pathogenesis of atherosclerosis. ED is a consequence of the harmful effects of risk factors of atherosclerosis on the vessel wall and is closely related to the number of risk factors, to their intensity and their duration. ED has been demonstrated in subjects with hypercholesterolemia, diabetes, hypertension, smoking, and in patients with atherosclerotic disease (coronary or peripheral). The involvement of risk factors in ED is also supported by results of intervention studies that showed regression of ED with treatment of risk factors. Improvement of ED may be achieved by elimination of risk factors, by substitution of natural protective endothelial substances, inhibitors of endotheliumderived contracting factors (ACE inhibitors), cytoprotective agents (free radical scavengers such as superoxide dismutase), lipid-lowering drugs (statins) or diet and physical exercise. All these data show that ED is reversible and by treatment of risk factors it is possible to restore vascular function. ED promotes progression of atherosclerosis and probably plays an important role in the development of thrombotic complications in the late stages of the disease. There are two groups of markers of ED: 1) disturbances of vessel-wall function – ↓dilatation capability 2) circulating markers of ED: – ↓NO availability, ↑endothelin - ↑Von Willebrand factor – ↓T-PA, ↑PAI – ↓Prostacyclins, ↑TXA2 - ↑Adhesion molecules (VCAM-1, ICAM-1, P-selectin) Using markers of ED it is possible to follow doseresponse or harmful effects of risk factors and the effects of preventive procedures on vessel wall function. Determination of ED also has important clinical implications. It was shown that ED is significantly and directly correlated to the occurrence of cardiac events increased as ED worsens.
Propionyl carnitine: not only a metabolic drug
G. BREVETTI (Italy)
Carnitine is a natural amino acid that plays a key role in the metabolism of skeletal muscle. It permits long-chain fatty acid oxidation and reduces the intracellular buildup of noxious metabolites. The latter function is particularly important under ischemic conditions when acyl CoA accumulates within the mitochondria and inhibits many enzymatic activities. In 1980 it was published that carnitine supplements improve cardiomyopathy due to carnitine deficiency, and the link to peripheral arterial disease was made by correlating the plasma levels of shortchain acetylcarnitine and walking capacity. Propionylcarnitine (PCL) is a carnitine derivative that provides additional substrates for energy production (in comparison with carnitine) and so supplements are more effective in improving exercise tolerance, walking capacity, and quality of life in patients with intermittent claudication. PCL is not only a metabolic drug; the pleiotropic effects of PCL are: – Endothelium-mediated vasodilatation – free radical scavenging – anti-inflammatory action (inhibits the synthesis of platelet activator factor from neutrophils) – endothelium-protective properties. In summary, PCL is an endothelium-dependent vasodilatator which inhibits PAF synthesis, reduces oxidative damage, reduces peroxidation, improves endothelial function, attenuates intimal hyperplasia following vascular injury, and reduces atheroslerotic lesions.
Infectious serology and PAD: how burdensome is the risk?
S. NOVO, I. MURATORI (Italy)
Peripherial arterial occlusive disease (PAOD) is recognized as a symptom of systemic atherosclerosis. Patients with PAOD, even in the absence of a history of myocardial infarction or ischemic stroke, have approximately the same relative risk of death from cardiovascular causes as do patients with history of coronary or cerebrovascular disease. The age-adjusted prevalence of PAOD is approximately 12 percent, and the disorder affects men and women equally. In many papers it was shown that persistent infections can promote proinflammatory, procoagulant, and proatherogenic environment and induce autoimmunity against vascular cells, so leading to an atherogenic process. There are many molecular mechanisms which lead to inflammatory changes, but the most visible for investigators are the increased concentration of different types of antibodies. In the end of the 20th century a correlation was shown between Chlamydia pneumoaniae infection and the occurrence of abdominal aortic aneurysm. Many of these patients presented a high concentration of IgG and IgM antibodies. Further observations shown that Herpes simplex virus and Chlamydia pneumoniae are able to initiate and accelerate the atheromathous process – this was demonstrated both in animals and humans. In hypersensitive patients with high concentration of SIgA and IgG against HSV and Chlamydia there was an 8.5-fold increased risk of stroke and 2.7-fold increased risk of cardiovascular events. All changes caused by micro-organisms can be divided into two groups: local and systemic. Local changes are related especially to dysfunction or endothelium injury and can be revealed as: – proliferation and migration of smooth muscles – local release of cytokines – inflammation – modulation and/or inhibition of prostaglandins – reduction in nitric oxide – expression and/or modulation of nuclear factor kB – modulation of apoptosis – increase in TNF alpha and metalloproteinases Systemic mechanisms are more complicated and manifest themselves as: – inflammation and increased blood levels of inflammatory cytokines – leukocytosis – induction of C-reactive protein and fibrinogen – alteration of hemostatic factor levels – hyperviscosity and hypercoagulability – autoimmunity (heat shock protein expression) – genetic polymorphism of CD 14 receptor There are very interesting results of a multicenter study of PAOD and Chlamydia pneumoniae, Helicobacter pylori, and Cytomegalovirus infections in young women with a several-fold increased CRP level. It was shown that increased level of IgA blood concentration is related to a twofold increased risk of PAOD for women with Chlamydia pneumoniae infections and 1.6 times for both Helicobacter pylori, and Cytomegalovirus infection. Finally it is still undetermined as to whether elevation of these inflammatory markers reflects the degree of underlying atherosclerosis or plaque vulnerability or rather results from some other environmental of infectious stimulus, or even has direct effects on platelet aggregation and coagulation. Ongoing future investigation will clarify the specific pathophysiologic relationships through which these markers correlate with adverse prognosies.
Peripheral arterial disease, inflammation and cardiovascular risk: does endothelial dysfunction provide a link?
G. BREVETTI, A. SILVESTRO (Italy)
Peripheral arterial disease (PAD) is associated with increased cardiovascular risk which, however, appears to be independent of classic risk factors and only partly explained by the expected association of PAD with coronary and carotid artery disease. Conversely, poor long-term prognosis of these patients is strongly related to severity of PAD and has been recently found to be associated with elevated plasma levels of inflammatory markers. A possible mechanism linking severity of circulatory failure in the affected limb and acute phase of proteins to cardiovascular risk could be endothelial dysfunction. Actually, when affected by inflammation and other injurious stimuli, endothelium may adopt a phenotype that, by predisposing to vasoconstriction, thrombosis, leukocyte adhesion, and smooth muscle proliferation, facilitates the formation and progression of atherosclerotic lesions. It is very interesting that acute maximal exercises amplified systemic endothelial dysfunction. PAD patients have a marked impairment in endothelial function, that in addition to classic risk factors is related to severity of the circulatory failure in the affected limb and with increased plasma levels of several inflammatory markers. Changes are observed not only in affected limbs. This suggests that endothelium, being a target that integrates the damaging effects of traditional and novel risk factors, may be a barometer for cardiovascular risk. Indeed in PAD patients, brachial artery flowmediated dilatation (FMD), a marker of endothelial function, is an independent predictor of future cardiovascular events. Even more importantly, FMD improves the predictive value of ankle/brachial index which is currently the most powerful prognostic indicator in PAD. What is missing is the demonstration that interventions specifically aimed at improving endothelial function protect against cardiovascular risk.
Role of oxidative stress and white blood cells in peripheral arterial disease?
S. SIGNORELLI (Italy)
Many cellular reactions can originate from ischemia, and this cellular damage has been called ”oxidative stress” (OS). OS has a crucial role as it is able to affect cell and vascular damage. Different authors have found: reduction of redox ability of cells, increase in release of free radicals from O2 increase of lipid peroxides, increase in neutrophil pooling, and endothelial cell damage. In peripherial arterial disease there was a higher level of direct and nondirect markers of oxidative stress, such as melonildhyaldehide and oxidized low density lipoproteins in comparison with controls. On the other hand in PAD patients lower levels of glutathione peroxidase enzyme were found. The imbalance between oxidative and redox status was stressed in PAD patients in a treadmill exercise. In fact there was a relationship between OS and cell damage, and this has been demonstrated by high release of cytokines as interleukin 1, 1B, and IL6, both with high levels of intercellular adhesion molecule 1 (ICAM-1). Moreover, there were higher levels of selectins (L,E,PS). More studies have been addressed at studying antagonism of the OS as a crucial key to ischemia and pathophysiology of PAD patients. Interesting results have been reached both in clinical events (ie, intermittent claudication, absolute free walking distance, skin condition and integrity, outcome of disease) and in endothelial markers (ie, reactive post ischemia / hyperemia markers of the OS, cell damage markers). Some metabolic drugs such as L-carnitine, increase the clinical performance of PAD patients and also cytokine and integrin release – this can be considered as an interesting therapeutic approach to antagonizing OS.
Inflammation in peripheral arterial disease: a predictor of disease progression?
J. J. BELCH (UK)
The atherosclerosis is a more complicated process which receives major contributions from inflammatory mechanisms. The main role in this process is played by white blood cells count (WBC) which is recognized as a predictor of the disease even in the normal range. Physical rolling of WBC in PAD is related to their adhesion and aggregation to the vessel wall – this is observed in patients with claudication and predestined to progressing of critical ischemia. The products released from WBC such as free radicals and proteases intensify oxidative stress and improve endothelial dysfunction. Insufficiency in nitric oxide production by endothelial cells leads to smooth muscle proliferation and degenerative changes. The physical obstructive effects of WBCs combined with oxidative stress generated by these cells and other mechanisms such a reperfusion have a potential deleterious effect in patients with peripherial arterial disease. All these result in poor vasorelaxants function and progression to critical limb ischemia. It was clearly documented that coexistence of inflammatory diseases improves oxidative stress and intensifies atheromatic changes. On the other hand, coexistence of rheumatoid disease with PAD can improve the mortality ratio, for instance 3 fold for rheumatoid arthritis or 4.5 fold for systemic lupus erythematosus. So there is a necessity to focus future studies on this area, and for new therapies not only focused on inflammatory disease but on prevention of atheromatic systemic changes.
ORAL COMMUNICATIONS
Outcome of conservative therapy in patients with severe intermittent claudication
J. AMIGHI, S. SABETI, O. SCHLAGER, M. FRANCESCONI, R. AHMADI, E. MINAR, M. SCHILLINGER (Austria)
This was a retrospective cohort study which aimed to asses the intermediate-term outcome of conservatively treated claudicants, and determine predictors for clinical improvement. The majority of patients remained clinically and hemodynamically stable. In 20% of the patients who improved clinically, hemodynamic changes were also present. Only a few patients worsened. The worst results were observed in female patients, diabetic patients, and in patients with initial ABI under 0.44. This study presents several limitations. It is not randomized, it is retrospective, and the patients did not do the exercise under supervision. However, it would be interesting to know which patients will not improve with conservative treatment.
Disease-specific quality of life analysis in intermittent claudication: is it really necessary?
T. MEHTA, I. CHETTER, A. VENKATASUBRAMA, K. MYLANKAL, B. RAY, P. McCOLLUM (UK)
The authors compared three disease- specific quality of life instruments (QOL) in a group of 67 patients with intermittent claudication which were Claudicant Scale (Claus), Kings College Vascular Quality of Life (VASCUQOL) and Sickness Impact Profile: Claudication Specific (SIPIC) and the general QOL scales like SF36 and EUROQOL. The correlation between disease-specific QOL measures and walking distance is high in the three specific tests. The CLAUS offers no advantage, but the VASCUQOL and the SIPIC are more useful than the generic tests to evaluate quality of life in patients with claudication.
Combination of high homocysteine levels and low ankle-brachial index predicts mortality
C. DIEHM, S. LANGE, H. DARIUS, R. HABERL, D. PITTROW, B.V. STRIZKY, J. R. ALLENBERG, G. TEPOHL, J. J. TRAMPISCH (Germany)
This is a study based in the German Epidemiological Trial on Ankle Brachial Index (GET ABI). It is an observational prospective 3-year study in 6880 unselected patients aged e 65 years. This study was created to determine the real incidence of peripheral arterial disease in the German population. The principal results of this study are no different from other epidemiological studies developed in other European countries. The incidence of peri – pheral arterial disease measured by the ankle brachial index was 18%. The incidence of PAD increases with the age, current smoking or past smoking, the presence of diabetes, or high homocysteine levels. Finally the author points out the premature mortality of patients with low ABI and high homocysteine level.
Noninvasive assessment of collateral circulation and capillary filtration
H. K. DEOL, L. SINGH, M. ASLAM, N. J. STANDFIELD (UK)
The authors describe a new noninvasive method to evaluate collateral circulations and capillary filtration in a group of patients with peripheral arterial disease (PAD) and diabetes mellitus (DM). They measured blood flow in the popliteal artery by ultrasound and total limb blood flow and capillary filtrations by optoelectronic plethysmography. In the patients with PAD there was an increase in total blood flow and in popliteal blood flow which can be attributed to the development of their collateral circulation. This increase was not observed in diabetic patients. Probably the alteration of the microcirculation which exits in diabetic patients is the reason for the lack of increase in blood flow. This method could help study microcirculation in PAD, but is not very useful in the clinical practice.
Treating claudication: angioplasty and exercise, not angioplasty or exercise
T. MEHTA, I. CHETTER, A. VENKATASUBRAMA, K. MYLANKAL, B. RAY, P. McCOLLUM (UK)
The authors compare two groups of patients with intermittent claudication due to angioplastiable femoropopliteal lesions. One group was treated with angioplasty (PTA) alone and the other was treated with angioplasty and a supervised exercise program (PTA+SEP). All the patients were evaluated 3 months later. In both groups there were improvements in the maximum walking distance, quality of life measured by SF36 test, and in the ankle-brachial index, but the increase was superior in the PTA+SEP group. Probably the first option for treating patients with intermittent claudication due to femoropopliteal lesions is exercise, reserving open surgery or endovascular treatments for some special cases. Obviously supervised exercise will improve the results. In any case, it is important to recommend exercise after any kind of vascular treatment.
The activation of the hemostatic system in PAD
P. GIOLINO (Italy)
There are no clear definitions of atherothrombosis. It may be defined as: – thrombus formation on an existing atheroscler tic plaque – or generalized progressive disease of large and middle-sized arteries that affects multiple vascular beds, including cerebral, coronary, and peripheral arteries. The classical view of thrombosis presents in two ways: platelet activation and coagulation cascade. However, contemporary observations show that the process is more complicated. Thrombosis is initiated by tissue factor. Thrombin triggers platelet activation. Platelet surface plays a central role in coagulation factor assembly and burst of thrombin generation. So the present observations distinguish three phases of coagulation: – initiation – priming – propagation. Analysis of the data from the Framingham Heart Study showed that atherothrombosis reduces life expectancy by around 8 to 12 years in patients aged over 60 years. In many other papers relationships were shown between intensification of PAD and high concentration of different products of thrombogenesis. It is important that all these disturbances are related to endothelial cell damage or dysfunction. So PAD should not be considered as a local disease, but rather as a clinical manifestation of atherothrombosis. These observations should prompt us to extend prescription of antithrombotic drugs.
LECTURES
Vascular disease in diabetes: epidemiology, pathophysiology, and treatment
M. A. CREAGER (USA)
The number of diabetic patients is increasing enormously, especially in developing countries. Atherosclerosis is the major cause (80%) of diabetic mortality (75% coronary, 25% CVA or PAD). Potential mediators of vascular disease (atherosclerosis) in patients with diabetes mellitus are:
1. abnormalities in endothelium, vascular smooth muscle, and platelet function
2. metabolic abnormalities:
• hyperglycemia
• increased free fatty acids
• insulin resistance hese mediators have their effect on the endothelial layer and cause vasoconstriction, inflammation, and thrombosis. These abnormalities contribute to the cellular events that cause atherosclerosis and subsequently increase the risk of adverse cardiovascular events. Agressive medical treatment that optimizes glucose control (insulin, metformin), achieves normal blood pressure (ACE inhibitors, â-blockers), corrects dyslipidemia (statins, fibrates) and prevents thrombosis (platelet function inhibitors) is necessary. SYMPOSIUM IUA/SFMV
Chairpersons: L. BOON (Belgium), I. QUÉRÉ (France)
From homocysteinuria vascular phenotype to mild homocysteinemia
I. QUÉRÉ (France)
Homocysteinemia is a rare constitutive metabolic disease but is treatable. It is defined by a plasma homocysteine concentration above 100 μmol/L, combined with a urinary excretion of large amounts of homocysteine. Homocysteinemia is the result of an enzymatic defect in one of the methionine metabolism pathways. The most common cause is a cystathionine â synthase (CBS) deficiency in the transulfuration pathway. It is characterized by high methionine and low cysteine levels and chronic intoxication disease. An impaired remethylation pathway may also occur, due to defects in methionine synthetase, in methylenetetrahydrofolate reductase (MTHFR), or in enzymes involved in the metabolism or transport of cobalamin. It is characterized by low methionine levels and an acute disturbance in stressful situations. Histologic vascular abnormalities in patients with homocysteinuria are at the level of large and medium-sized arteries, with focal intimal and medial fibrosis and proliferation of perivascular connective tissues surrounding small arteries. The intima/media thickness measured by echography is much higher than in controls. Hyperhomocysteinuria, whatever the type of enzymatic deficit, leads to an increased risk of venous and arterial thrombosis. In a cohort of 629 patients with CBS homocystinuria, 25% had thrombosis before the age of 30 years, (49% arterial thrombotic events and 51% venous thrombotic events), In all the published cohorts, venous risk of thrombosis is high, even in patients without other risks of VTE, mutation of factor V for example. Treatment of homocysteinuria by vitamin B6 (pyridoxine) reduces the risk of thrombosis. In a cohort of 158 patients, 50% of them were responders to treatment with vitamin B6, and 50% were not. Only 17 thrombotic events were observed during follow-up instead of 112 expected without treatment. Despite effective treatment with vitamin B6, the thrombotic risk remains 5 fold superior to the risk observed in the general population. The prevalence of homocystinuria is underestimated and is probably closer to 1/30 000 live born babies than the previous expected prevalence of 1/ 300 000. This may be due to mild phenotype with predominant vascular thrombotic phenotype diagnosed in the adulthood.
Genetics and mechanisms of aortic aneuryms: from Marfan to isolated familial aneuryms
C. BOILEAU (France)
Thoracic aortic aneuryms may have a mendelian inheritance in Marfan (MFS) and Marfan-like syndromes (MFLS). MFS is diagnosed only by a clinical approach, screening for eye, skeletal, cardiovascular, pulmonary, skin, and integument abnormalities. MFS is associated with mutations of the FBN1 gene located on chromosome 15 and coding for fibrillin 1. More than 600 mutations have been identified in complete and incomplete forms of MFS, each family having its own mutation. Fibrillin 1 mutations have also been identified in various overlapping disorders, among which are isolated forms of aortic aneuryms. Fibrillin-1 is the major protein component of microfibrils, that are closely associated with elastin fibers in elastic tissues such as the aortic media. Pathogenic steps of the formation of aortic aneuryms have been identified in the mouse model with fibrillin 1 mutations and a Marfan phenotype. Probands (n=81) presenting with isolated thoracic aortic aneuryms were investigated and 16 of them were familial cases. Among these, 10 were undiagnosed complete or incomplete Marfan syndromes but 6 were a pure familial form of aortic aneuryms (FAA). FAA is an autosomal dominant disease with incomplete penetrance. Three different genes were mapped. The identification of these genes will provide further information about the pathogenic mechanisms of aortic aneuryms.
Genetics of lymphedema
L. BOON (Belgium)
Isolated primary lymphedema is associated with a family history in 35% of cases. It may be either congenital, with a puberty onset or with a later onset. Several mutations have been identified in the vascular endothelial growth factor receptor 3 gene (VEGF-R3) in primary congenital lymphoedema families. These mutations are responsible for an nonfunctional receptor, unable to bind its ligands (VEGF-C and VEGF-D). VEGF-R3 is a membranous receptor, specific to lymphatic vessels. Mutations in the gene FOXC-2 are responsible for lymphedema distichiasis phenotype. FOXC-2 is a transcription factor implicated in the signalling pathway of VEGF-R3. Lymphedema hypotrichosistelangiectasia is characterized by lymphedema often located in a leg, beginning between 0 and 15 years, telangiectasia mostly on the palms and the soles and hypotrichosis of the scalp, and sometimes of the eyebrows and of the eyelashes. Mutations in the SOX 18 gene have been identified in the 3 families who were investigated. These mutations can be both recessive or dominant. SOX 18 is encoding for a transcription factor, which has an established role in hair and blood vessel development in mice. It is also necessary for the development and/or maintenance of lymphatic vessels, probably by an interaction with the VEGFR3 signalling pathway.
Chairpersons: C. SETACCI (Italy), A. WILLFORT (Austria)
Enoxaparin for cerebral artery dissection
M. MARIETTA, S. VALLONE, M. COBELLI, L. FACCHINI, S. POZZI, M. BERTESI, L. MAVILLA, G. TORELLI (Italy)
Cerebral artery dissection is a rare entity, and its treatment is still a matter of debate because of the lack of trials directly comparing either anticoagulants with antiplatelet agents or any treatment with placebo. The author presented his experience in 9 cases treated with enoxaparin at therapeutic doses for 3 weeks and at prophylactic doses for 3 more weeks. A magnetic resonance angiogram was then performed showing complete recanalization in 6 patients and partial recanalization in 3. As very few literature data are available at the moment the author suggests enoxaparin as a possible treatment, being a safe and useful therapy for thrombosis accompanying cerebral artery dissection.
Arterial remodeling and hemodynamics in carotid stents
A. WILLFORT, R.A. AHMADI, D. GRUBER, M. E. GSCHWANDTNER, A. HAUMER, M. HAUMER, H. EHRINGER (Austria)
After the experience on coronary stents showing positive remodeling (due to stent expansion) and negative remodelling (due to in-stent intimal hyperplasia), the author designed this study for carotid stents. A total of 121 stented carotid arteries were included in the study. Duplex ultrasound was performed before the procedure (plaques were assigned to three different groups: soft, fibrous and calcified), the day after and at 3, 6, 12, and 24 months. They measured the stent diameters (proximal, distal and medium), the maximal neointimal thickness and hemodynamic parameters. They observed stent expansion over the 2 years, most marked on the middle stent area and related to the type of preinterventional plaque (maximal for soft and minimal for calcified plaques). Neointimal thickness had a marked increase during the first year and a minimal increase thereafter. These interactions resulted in a dominance of negative remodeling with an increased flow ratio during the first year, followed by a tendency to decrease due to stent expansion thereafter. This might contribute to the good midterm outcome of carotid stenting, especially in noncalcified plaques.
Influence of HbA1c on healing of carotid stents
A. WILLFORT, R. A. AHMADI, A. GESSI, M. E. GSCHWANDTNER, A. HAUMER, W. LANG, E. MINAR, S. ZEHETMAYER, H. EHRINGER (Austria)
A total of 112 patients were followed prospectively after carotid artery stenting (CAS) over a period of 24 months. They were assigned to three groups according to their diabetic condition: group A nondiabetic subjects and group B diabetic subjects, who were subdivided into B1 (HbA1c<6.5%) and B2 (HbA1>6.5%). The groups were homogenous concerning risk factors and residual stenosis on angiograms. The maximal thickness of the layer between the stent and the lumen was measured at duplex follow-up and analyzed. Patients in group B2 differed significantly compared with B1 and A in respect to the maximal thickness of neointima and the time of its ingrowth. Initial hyperglycemia seems to be a predictor of more pronounced neointimal proliferation after CAS; therefore, a strict optimization of the hyperglycemic state should be aimed for in this kind of patient.
Carotid endarterectomy in Sapphire-eligible high-risk patients
G. MOZES, T. M. SULLIVAN, D. R. TORRES-RUSSOTTO, T. C. BOWER, T. L. HOSKIN, S. SAMPAIO, P. GLOVICZKI, J. M. PANNETON, A. A. NOEL, K. J. CHERRY (USA)
This group from the Mayo Clinic presented a retrospective analysis of carotid endarterectomy (CEA) in high-risk patients, who could be included in the Sapphire trial. With an analysis of 776 CEA, 323 (42%) in high-risk patients, there was no statistical different in the stroke (1.4%) and mortality (0.3%) rates when comparing high-and lowrisk patients. The authors conclude that high-risk patients, as defined in CAS trials, can undergo operation with very low stroke and death rates.
SYMPOSIUM. IUA/WORKING GROUP ESC ON PERIPHERAL CIRCULATION
Chairpersons: D. L. CLEMENT (Belgium), P. RIZZON (Italy)
Arterial stiffness: how to evaluate it
V. VLACHOPOULUS C. STEFANADIS (Greece)
Several theoretical models are available to evaluate arterial stiffness; two models are the most popular. While the Windkessel model is the simplest way to assess the cushioning function of arteries, the most realistic model of the arterial system is a simple tube with one end representing the peripheral resistance and with the other end receiving blood in spurts from the heart. The methods can assess arterial stiffness on three levels:
1. local determination:
● invasive
– aortic catheter: pressure and diameter measured at the same site
– transbrachial ultrasound
– transthoracic echocardiography
● noninvasive
– transesophageal echocardiography
– Wall Track system
– Tissue Doppler imaging
2. regional determination
● invasive
– pulse wave-velocity measurement by simultaneous intra-arterial recording
● noninvasive
– Complior
– Sphygmocor
– Wall tracking system
– Simultaneous ultrasound recording
– Cine MRI
– Timing of Korotkoff sounds (QKD interval)
3. systemic determination
● noninvasive
– Sphygmocor-applanation tonometry
– Diastolic pulse contour analysis
– Photoplethysmography
Devices and methods are based on measurement of pulse transit time, analysis of the arterial pressure pulse, or on direct stiffness calculation using measurements of dimensions and pressure. The most widely used of these methods are accurate and reproducible enough to allow understanding of arterial mechanics and their impact on cardiovascular function.
Modification of arterial stiffness: is it feasible
C. VLACHOPOULUS (Greece)
Arterial stiffness has been identified as an independent predictor of cardiovascular risk. Modification of arterial stiffness is an important target for prevention and therapy. Determinants of arterial stiffness are genetics, age, height, blood pressure, and heart rate. Alterations in last two determinants are possible in a pharmocological and nonpharmacological way. – Pharmacological modifications: – Antihypertensive drugs: ACE inhibitors, angiotensin receptor blockers, calcium channel blockers, nitrates and NO donors, â-blockers – Oral antidiabetic drugs – Hypolipidemic drugs – Others: ALT-711 – Nonpharmacologic modifications: – Reduction in obesity: weight reduction results in a reduction of arterial stiffness independent of the type of diet – Quitting a sedentary lifestyle and starting regular exercise: the more one trains, the less stiff the arterial wall, especially with aerobic training (walking) rather than muscular strength training which causes endothelial damage – Cessation of smoking (cigarettes and cigars): causes endothelial dysfunction with an acute effect after 1 minute; the chronic effect is unknown – Nutrition: diminish salt intake, higher intake of foods with antioxidant properties (flavonoids, garlic, vitamin C, chocolate, fruits, tea), reduction of caffeine.
ORAL COMMUNICATIONS
Chairpersons: R. MARTINI (Italy), T. OTHA (Japan)
Intermittent compression pump for nonhealing wounds in patients with limb ischemia
V. M. MONTORI, S. J. KAVROS, E. E. WALSH, T. W. ROOKE (USA)
The Aircast Arterial Flow® system provides intermittent pneumatic compression of the calf in order to help prevent and reduce the complications of poor circulation. Compression is rapid, graduated, and sequential. The rapid inflation produces shear stress within the vasculature and may induce a biologically mediated vasodiatory effect. The graduated sequential compression accelerates venous velocity. This system may represent a rescue treatment for patients unwilling or unable to undergo a limb amputation, but little is known about its safety and its efficacy in ischemic wounds. This retrospective single-center study included 101 patients with wounds in the lower extremity with ulceration, from various etiologies (multifactorial 52%, arterial 36%, small vessel disease 7%). Sixty-four percent of the patients were diabetic, and 25% had a history of amputation. TcPO2 was below 20 mm Hg in 60% of the cases. Complete wound healing was achieved in 40% of patients with a TcPO2 < 20 mm Hg and in 47% of the patients with a TcPO2 between 20 and 30 mm Hg. Seven patients discontinued the treatment by the Aircast Arterial Flow® system because of pain. Wounds healed with a median time of 14 weeks of treatment. These results have to be confirmed in a prospective randomized study.
