Analysis of the various procedures used in great saphenous vein surgery in the Czech Republic and benefit of MPFF at a dose of 500 mg to postoperative symptoms
Václav JEDLIČKA,
Jan WECHSLER,
Jan KALAČ
Czech Republic
SUMMARY
The aim of this clinical study was to compare the intensity of postoperative pain using a 10-cm Visual Analog Scale (VAS), a quality-of-life questionnaire (CIVIQ), and a patient diary between two groups of patients, consisting of:
• a treatment group: patients who underwent a stripping procedure of the great saphenous vein (GSV), and were treated with MPFF at a dose of 500 mg®* 14 days before and 14 days after the operation, 2 tablets 500 mg/day;
• a control group: patients who underwent stripping of the GSV, but were not treated with MPFF at a dose of 500 mg®.
In addition, the two groups were also compared for the size of postoperative hematoma, analgesic consumption, and for the incidence of other symptoms associated with chronic venous disease (edema, tired and heavy legs, cramps, sensation of itching), using the VAS scale. Lastly, overall efficacy of the treatment was assessed.
The present trial included 181 patients from 15 medical centers throughout the Czech Republic. High ligation and partial stripping of the GSV in one lower limb was performed in all patients (short stripping from groin to knee). Patients were randomly assigned either to the treatment group (92 patients) or to the control group (89 patients). The degree of pain and the patient’s condition were evaluated by the physician 14 days prior to the surgery (D- 14), then 7 days (D7) and 14 days (D14) after surgery. Results indicated that MPFF at a dose of 500 mg reduced the intensity of postoperative pain, which resulted in decreased consumption of analgesics. The size of postoperative hematoma was significantly smaller in the treatment group compared with the control group (P<0.001), and associated symptoms of CVD and quality of life were significantly better in this group.
Effective phlebotropic drugs, like MPFF at a dose of 500 mg, administered to patients 14 days before and 14 days after stripping surgery may improve postoperative morbidity.
*also registered as Alvenor®, Ardium®, Arvenum 500®, Capiven®, Detralex®, Elatec®, Flebotropin®, Variton®, Venitol®, Viatec®.
INTRODUCTION
Chronic venous disease of the lower limbs is a common disorder.1,2 Results of an epidemiologic survey in the Czech Republic show that 18.6% of the general population suffers from at least 3 of the symptoms attributed to chronic venous disease (CVD): pain, heaviness in the legs, and a sensation of swelling.3 Most of the CVD patients in this trial were untreated.3 Varicose veins (VV) are a frequent manifestation of this disease. Their prevalence in a recent epidemiological survey performed in Europe and using the clinical, etiological, anatomical, and pathophysiological (CEAP) classification,4 amounted to 40% in women and 20% in men.5
Until now, stripping surgery has been the procedure most often used for removing VV. Stripping surgery aims to eliminate venous reflux in the superficial venous system whilst the patient is in the standing position6 by eradication of the refluxing part of the superficial veins. Thus, a brief preoperative Doppler investigation is usually performed in order to locate the section affected by valvular incompetence. Despite excellent postoperative results of stripping surgery and very low complication rates, morbidity due to hematoma in the thigh and postoperative pain and edema are reported.7
The anti-inflammatory effect of MPFF at a dose of 500 mg has been demonstrated in a number of studies.8 Therefore, MPFF at a dose of 500 mg may improve major symptoms seen after surgery, particularly pain, and traumatic signs such as hematoma.
AIM OF THE STUDY
The primary objective of the study was the evaluation of postoperative symptoms and signs in two groups of patients undergoing varicose vein stripping of the great saphenous vein (GSV): a treatment group receiving 1 month of treatment with MPFF at a dose of 500 mg, and a control group with no MPFF at a dose of 500 mg treatment.The secondary objective of the study was to report on methods of stripping used for the resection of varicose veins and analyze their possible impact on postoperative morbidity.
STUDY DESIGN
This study was an open-label, multicenter, prospective, randomized trial conducted by 15 vascular surgeons in the Czech Republic. One hundred eighty-one patients were evaluated (92 in the treatment group, 89 in the control group) who needed to undergo surgical treatment (stripping), regardless of their participation in this study.
Duration of therapy with MPFF at a dose of 500 mg in the treatment group was 1 month (14 days prior to and 14 days after surgery), at a dosage of 2 tablets of MPFF at a dose of 500 mg a day.
Assessment visits were performed as follows: 14 days prior to surgery (D-14), 7 days (D7) and 14 days (D14) after surgery.
INCLUSION CRITERIA
Patients had to be between 18 and 60 years of age, scheduled to undergo GSV partial stripping as follows: high ligation + a short stripping from groin-to-knee, procedure to be performed on one lower limb without sclerotherapy and without ligation of perforating veins. One of the following procedures could be used: conventional stripping (using the Babcock stripper), invagination stripping, cryostripping, phlebectomy.
Postsurgical compression:
• Compression stockings and bandages were allowed post-surgery.
Additional conditions:
• Treatment with any other phlebotropic drug during the 4 weeks prior to inclusion was unauthorized;
• Existence of primary VV associated with venous reflux had to be confirmed by duplex ultrasonography.
Statistics:
• At baseline, the comparison between groups was tested using the Student’s t-test; and Mann-Whitney’s U Tests were performed for comparison between the control and treatment groups of quantitative variables. A value of P<0.05 was considered significant.
INVESTIGATION AND EVALUATION
A 10-cm visual analog scale (VAS) was used to evaluate pain and symptoms in patients with CVD in visits to the physician at D-14, D7, and D14. CIVIQ, a 20-question quality-of-life questionnaire dedicated to CVD, was filled in at D-14 and D14.
Patient’s diary: the pain dimension of the CIVIQ (4 questions concerning pain, see Table I), 10-cm visual analog scale (VAS), and consumption of analgesics were self-assessed by patients on a daily basis.
The physician evaluated the size of the hematoma at D7 and D14 visits using transparent adhesive tape to outline the hematoma and measure it (a computerized – Hematoma Analyser was used for the hematoma assessment).
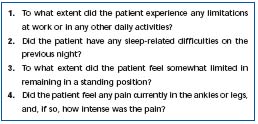
Table I. Four questions related to pain in the CIVIQ (pain dimension).
RESULTS
1) Pain
In both the treatment and control groups, patients reported relief from the pain they complained of prior to surgery. In the treatment group, better pain relief was reported, namely during the first 7 post-surgical days, with a decrease in pain intensity by almost half (43%).
Moreover, a daily greater improvement trend and complete pain relief were seen in the treatment group, compared with the control group (Figure 1).
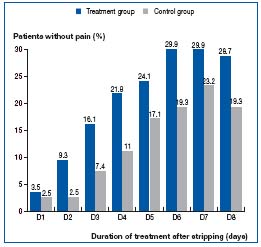
Figure 1. Complete resolution of pain after surgery.
Slower regression of postoperative pain in control patients was also manifest by a higher consumption of analgesics. A significant difference was observed between the two groups in terms of analgesic use from D4 since 4-times as many control patients required analgesics (Figure 2).
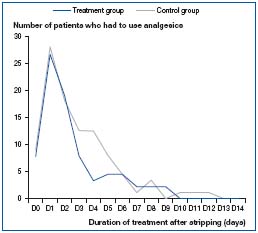
Figure 2. Decrease in the consumption of analgesics.
2) Hematoma
On D7, control patients showed a larger hematoma (131 cm2 on average) than the treated ones (110 cm2, P<0.001) (Figure 3).
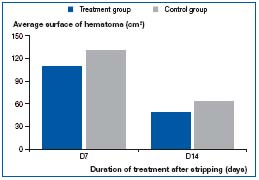
Figure 3. Decrease in the area of hematoma.
3) Quality of life
Regarding daily quality of life on the shortened CIVIQ (pain dimension only), a better improvement in each of the 4 items was reported in the treatment group compared with the control group (Figure 4).
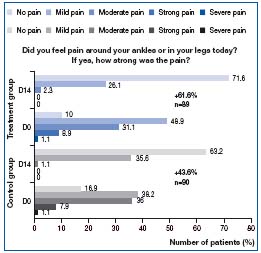
Figure 4. Evaluation of daily quality of life related to pain.
By the end of the study (D14), quality of life on the 20-item CIVIQ was rated as better by 21% of patients in the treatment group versus only 3% of patients in the control group.
4) Other symptoms related to chronic venous disease (CVD)
Patients in the treatment group also reported improvement in other symptoms of CVD: lower-limb edema decreased in 84%, sensation of heaviness in the legs in 89%, and itching in 92% of patients in this group. In this last group, patients reported early relief from lower-limb fatigue and cramps, starting on the first postoperative day. Improvement in all symptoms and signs was significantly better in the treatment group compared with the control group (P<0.001).
5) Multifactorial analysis of surgical procedures
A total of 181 patients underwent surgery, 28 of whom were in the hospital outpatient department. One hundred fifty-three patients were hospitalized, representing 85% of all included patients. Average hospital stay was 2 days (range: 1-6 days). Surgery was performed under general anesthesia in 139 patients. Other types of anesthesia used were local anesthesia in 3, epidural in 9, and spinal anesthesia in 33 patients. Based on records from the patients’ diary, the type of anesthesia did not have any effect on total pain in both groups of patients.
Table II shows that the majority of the patients were over 40 years of age (60.9%) and consequently at risk for thrombogenic complications. Data on this type of complication in the postoperative period after stripping, as well as in the long term, are lacking in the Czech Republic. Such complications in predisposed patients are known to increase the costs of treatment in the absence of preventive management, even in case of a minimally invasive procedure (Table III). Because a substantial percentage of the study population (34.3%) was considered at risk for thrombogenic complications (over 40 years of age, receiving hormonal therapy, presenting with VV, undergoing surgery, etc), lowmolecular- weight heparins (LMWH) were administered to them, although use of such LMWH is very low in standard practice. Administration of LMWH did not increase the size of the post-surgical hematoma.
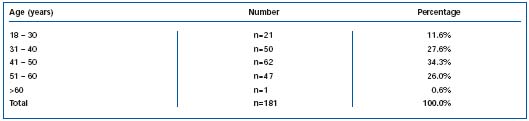
Table II. Classification of patients by age.
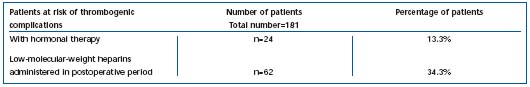
Table III. Administration of low-molecular-weight heparins.
In accordance with the study protocol, the following resection procedures had to be recorded by the investigator: high ligation associated with partial trunk stripping just below the knee and single leg resection procedure excluding any associated sclerotherapy, and excluding perforator vein ligation. The techniques that could be used for this surgery were the following: conventional stripping (with Babcock’s stripper), stripping by invagination, pin-stripping, cryostripping, and phlebectomy, by means of either exoluminal or endoluminal stripper, with the stripper pulled back in one of these two possible directions: from groin to knee or from knee to groin. Whether tributary stab avulsion was performed or not had to be reported by investigators. If tributary stab avulsion was performed, the location of stab avulsion (thigh, calf, medial side, lateral side) as well as the type of device used (hook, Trivex®, needle, mosquito forceps, other) and the time of stab avulsion (before or after the vein stripping) had to be recorded. All surgical techniques used in the present study are listed in Tables IV, V, VI. The invagination stripping technique was used the most often (70.2%). Only 28.7% of patients underwent the conventional stripping procedure.
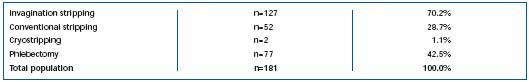
Table IV. Type of surgery performed in the present study in the Czech Republic.
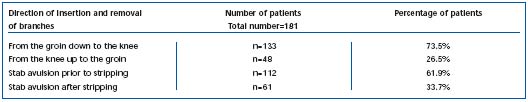
Table V. Effect on pain according to various directional insertions of the stripper.
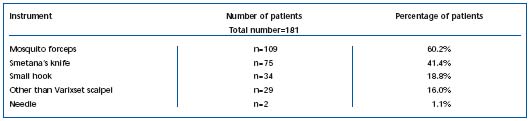
Table VI. Type of instrument used.
Statistically less pain and smaller hematoma size were reported by patients who had their VV stripped by invagination.
Of the 127 patients who underwent stripping by invagination, only 67 (48.2%) needed to take analgesics at D1 (all patients took analgesics at D0, just after being operated on) versus 68% of those stripped with other procedures. Direction of pulling stripper and time of stab avulsion are described in Table V. Among the other resection procedures used, the mosquito forceps caused fewer traumas than Smetana’s knife (Table VI).
Patients who underwent stab avulsion before the stripping experienced less postoperative pain than those with stab avulsion after stripping. Similarly, patients in the treatment group reported significantly less pain after surgery than patients in the control group (treatment effect, P<0.05).
Compression therapy is an integral component of postoperative management. Compression stockings and compression bandages are commonly used in poststripping. In this study, the medium-compression bandages were used in a majority of patients, ie, a total of 132 (73%), and elastic stockings were used in only 49 patients (27%). Short-compression bandages can be indicated after this type of surgery. However, due to their cost, they were only used in a small percentage of patients in the present study. Hematoma size proved to be significantly smaller in those patients who received compression stockings postoperatively, rather than bandages.
DISCUSSION
Varicose veins in the lower extremities should not remain untreated in the long term since the venous reflux they induce is known to damage adjacent tissues. This can result in further complications such as skin pigmentation, dermatitis, and lastly, the most advanced stage represented by crural venous ulcers.9-11 Phlebotropic drugs are of benefit to symptoms in all stages of CVD insofar as they decrease pain generated by endothelium-mediated activation due to venous stasis.12 Whenever VV appear, they should be treated by surgery6 in combination with pharmacotherapy. As early as the year 500, BC Hippocrates recommended making multiple punctures in varicose veins. In the 2nd century, AD Galen defended the removal of varicose veins using a small hook. In the 16th century, Amboise Paré recommended ligation and excision of varicose veins. In 1884, Madelung performed a long incision on the inner aspect of the leg and removal of the entire GSV. In 1905, Keller attempted to perform venous stripping by inserting a curved wire through the venous lumen. In 1906, Charles May used an extraluminal stripper to loop the vein. In 1907, Babcock described a rod-like stripper with a cylinder pin at one end. The development of the surgical technique has progressed very rapidly up to the presentday concept, which stipulates the removal only of the functionally incompetent vein and is associated with the best cosmetic result. Although the stripping procedure produces very good postsurgical results with few complications7 (postoperative hematoma in the thigh, edema, and pain). It appears that an effective phlebotropic agent can help to decrease this morbidity. Despite the recommendations by many scientific societies, prevention of thrombogenic complications is not considered in all cases. The reasons for this might be the additional costs such prevention can imply, and concern about the large postsurgical hematoma that LMWH can cause. The results of the present study demonstrated that the prevention of thrombogenic complications by LMWH does not increase the size of postoperative hematoma.
Regarding the different stripping procedures used, it appears that hematoma size was smaller after use of a mosquito forceps, removal of venous branches prior to stripping, and use of compression stockings. Patients reported less pain following the invagination stripping procedure compared with other procedures.
Patients in the MPFF at a dose of 500 mg treatment group had smaller hematoma and a lower consumption of analgesics. These patients also experienced a significant improvement in symptoms of CVD as well as in qualityof- life parameters. The findings of this study show that better results were obtained by administering MPFF at a dose of 500 mg 14 days prior to surgery and 14 days postsurgery. The administration of a phlebotropic agent, such as MPFF at a dose of 500 mg, can be helpful in mitigating postoperative pain and hematoma after stripping of the GSV.
Results of this study were first presented at the Phlebology Congress held in Hradec Králové, from 21 to 22 October, 2004.
This article is a translation of the original article published in the journal Rozhl Chir: Veverková L, Jedlička V, Wechsler J, Kalač J. Analysis of surgical procedures on the vena saphena magna in the Czech Republic and an effect of Detralex during its stripping [in Czech]. Rozhl Chir. 2005;84,410-416. Published here with the kind permission of Dr Tomáš Polák.

REFERENCES
2. Strejček J. Prevalence of chronic venous insufficiency in patients coming to the general practitioner and results of the treatment by selected venoactive drug (in Czech). Praktická flebologie XII. 2003;1:3-11.
3. Puchmayer V, Roztocil K. Venous diseases (in Czech). Praktická angiologie. Triton 1, first edition. 2000:115-164.
4. Porter JM, Moneta GL, and an International Consensus Committee on chronic venous disease. Reporting standards in venous disease: an update. J Vasc Surg. 1995;21:635-645.
5. Rabe E, Pannier-Fisher F, Poncar C. Bonn Vein study: epidemiologic study on the prevalence and risk factors of chronic venous disease. Paper presented at the 20th World Congress of the International Union of Angiology, New York City, April 9-14, 2002.
6. Perrin M. Surgical repair of varicose veins of the lower limbs by saphenous stripping (in French). Ann Chir. 1997;51:735-744.
7. Creton D. Conventional stripping: techniques, complications, results (in French). In: Kieffer E, Bahnini A. Chirurgie des veines des membres inférieurs. AERCV, Paris; 1996:124-143.
8. Lyseng-Williamson A, Perry CM. Micronized purified flavonoid fraction. A review of its use in chronic venous insufficiency, venous ulcers and haemorrhoids. Drugs. 2003;63:71-100.
9. Jantet G and the RELIEF Study Group. Chronic Venous Insufficiency – Worldwide results of the RELIEF Study. Angiology. 2002;53:245-256.
10. Heather Clarke G, Vaskedis SN, Hobbs IT, Nicolaides AN. Venous wall function in the pathogenesis of varicose veins. Surgery. 1992;111:402-408.
11. Torma N, Frankovičová M, Kubíková M, et al. Komplikácie pri operáciach varixov dolných končatín. Praktická flebologie. 2001;1-2:54-56.
12. Dormandy J-A. Microcirculation in venous disorders: the role of white blood cells. Inter J Microcirc Clin Exp. 1995;15:3-8.
