Lipedema, lymphedema, lipohypertrophy, and obesity: how do we differentiate?
Erika Mendoza, PhD
Vein Office, Wunstorf, Germany
ABSTRACT
Lymphological and fatty tissue disorders of the legs are increasingly tying up capacities in the health care system. This is related to the increase in obesity disease to almost endemic proportions in our society. Although the term lipedema was coined in the 1950s, it has only now become really well known. Women with lipedema suffer from symmetrical and disproportional fat deposition on both legs, accompanied by tenderness or strong pain especially on touch. Over 50 years, this condition has been underdiagnosed. Women with lipohypertrophy (same fat disproportion without pain) fear they suffer from lipedema and are misguided by false information, claiming treatment, as well as liposuction reimbursed by health care systems. Affected women suffer greatly from misinformation but also from overdiagnosis. The aim of this work is to make differential diagnosis easier for the health practitioner. On the basis of descriptions on visual inspection and palpation of the affected legs, the differential diagnosis is explained here, supported with many pictures. As a result, differentiation of the entities lipedema, lipohypertrophy, obesity, and lymphedema and their mixed forms is made easier for health practitioners in their daily work. Many studies are still needed to better understand the entity lipedema, and efforts are underway to change the name to avoid misunderstandings, as the condition “lipedema” does not seem to have water in the fatty tissue.
Introduction
Obesity, disproportion between abdomen and extremities (lypohypertrophy), and fat tissue pain are conditions that particularly affect women.1-6 It is possible that women have a genetically disposed capacity to store energy in the leg and gluteal fatty tissue.2 This might be an evolutionary selection criterion, as these fatty tissue deposits help in nursing a baby during hunger episodes (author’s speculation). These days, obesity is endemic in rich countries, where we do have fridges to prevent us from having weather-dependent hunger. Perhaps this also explains the yo-yo effect after diets, eg, during periods of hunger, the body “remembers” hunger periods from 10 000 years ago and is conditioned to store any food, as soon as it is available (author’s speculation). And this is exactly what happens after a diet, especially in women, and it is hard to overcome (author’s speculation).
In modern times, societal beauty standards show models that are slim and have perfect legs; thus, women often consider their legs to be part of their beauty and sex appeal. Thus, fat deposition on the legs is disturbing for women; they feel undesirable themselves and are surrounded by women held up as “wonderful” in the media. This makes the problem of obesity and disproportion not only an issue of health but also a complex issue involving psychology and self-acceptance.3
Independent of these disproportion and obesity problems, there are 2 clinical pictures that are very closely related to those described above and that can easily be confused; these are lipedema and lymphedema. Even though first described in the 1950s,7 it wasn’t until 2000 that interest was focused on knowledge of the condition lipedema.2 Parallel to this, we’ve had a pandemic increase in obesity since the late 20th century, contributing to obesity-related lymphedema as well as asymptomatic lipohypertrophy, increasing confusion.
The term lipedema suggests an edema component. This is reinforced by the fact that compression reduces the pain.1,2,6 A lot of investigation is needed to find the real reason for the pain in the affected women; there is very probably a high inflammatory component.1,4 The suggestion that manual lymphatic drainage is necessary in lipedema is derived from the misleading name.2
The differential diagnosis is even made more difficult by incorrect information spread through social media, suggesting that disproportion (ie, lipohypertrophy) equals lipedema, that lipedema inevitably causes psychological harm to the affected women, and that increase in body weight is unavoidably associated with lipedema. This places affected women in a helpless and hopeless situation. They approach the health care system in desperate need of help.1-3
A lot of work is needed to address this misleading information with 2 goals. One aim is to provide health care workers with information about these conditions, empowering them to support affected women in their concerns. The other is to correct public opinion with true information about the conditions lipedema, lipohypertrophy, lymphedema, and obesity, especially with an aim to correct confusion about the following: i) lipedema and obesity are often concomitant, but not related to each other; ii) obesity increases the disproportional shape of lipedema, but is not caused by lipedema1,2; iii) psychological disease is present in 80% of women before lipedema symptoms such as pain in the legs appear3; iv) psychological therapy reduces the pain of lipedema3; v) pain levels can be influenced by a ketogenic diet4; and vi) wearing compression garments during sport activities reduces the pain in lipedema.5
This article aims to provide tools to help easily distinguish the following: i) lipedema; ii) lipohypertrophy; iii) lymphedema; and iv) obesity of the legs. The diagnosis of these 4 entities is based on medical history, visual inspection, and palpation. Further investigation, such as with duplex ultrasound, is only helpful as an adjunct, to detect the extent of the edema and to exclude concomitant venous disease.1,2,6
Definitions of lipohypertrophy, lipedema,
lymphedema, and obesity with leg deformity
lymphedema, and obesity with leg deformity
Lipohypertrophy is described as symmetrical, disproportional deposition of fatty tissue on the legs and/or arms, respecting hands and feet, with a slim waist.1,2,6 The clinical picture is possibly hereditary.1,8 The women do not feel pain in the fatty tissue on touch or on movement.2Compression holds the disproportional, often smooth, tissue together and gives a better shape. During sports, compression avoids wobbling.
Lipedema has an optical presentation like lipohypertrophy, but with additional tenderness to the touch and sensitivity to pressure in the increased fatty tissue.1,2,5,6 In other words: a painful, symmetrical increase in fatty tissue on the legs and arms, with a slim waist.1,2,6 The condition seems to be hereditary. Classification into stages has been abandoned in some countries, as they were merely morphologic, not reflecting the pain intensity.1,2 The volume and shape of lipedema legs is mostly influenced by the degree of concomitant obesity, not by the lipedema itself.
Lymphedema is characterized by an alteration of the lymphatic drainage pathways, so that tissue-lymph is not drained physiologically, resulting in congestion and edema of the region.9 Lymphedema can be congenital, with early or late onset, can appear without any apparent reason, or as a result of an injury (trauma, surgery, radiotherapy).9 Currently, one of the most common causes of lymphedema is obesity, which delays the drainage of lymph via the groin and retroperitoneum and is often accompanied by a lack of exercise.10 On touch, the subcutaneous fatty tissue is consistent, not wobbling when moved back and forth, pressure on the skin creates a dent (like in a short-crust pastry), which remains for a few seconds. In an advanced degree of lymphedema, the accumulation of protein in the tissue increases and fibrosis of soft tissues occurs, then the texture changes from soft to hard or “stony” and only leaves a slight impression after half a minute of hard pressure.9
Lymphedema is divided into 3 stages, as follows: i) Grade I, reversible overnight; ii) Grade II, not spontaneously reversible; and iii) Grade III, with fibrosis and tissue sclerosis.9
Obesity with leg deformity could be described as extreme degrees of obesity causing deformities of the legs with dents, furrows, and dewlap formation. In these cases, the fatty tissue is distributed harmonically on the whole body. There is no pain on touch in the fatty tissue.1,2 Frequently, these women have leg pain due to other obesity-related illnesses, such as knee osteoarthritis, hip disorders, fascial pain, and muscle pain.
Diagnosis
Lipedema and lipohypertrophy
Visual inspection of lipedema and lipohypertrophy
Both conditions look similar, which is why their visual inspection is described here together. They differ only according to palpation findings. They can affect the entire leg and arm or only some parts, always excluding hands, abdomen, thorax, and feet.
Both conditions only affect women, and the appearance is always symmetrical.1,2 These 2 diagnoses cannot be distinguished by visual inspection alone, as their appearance is identical.
In women of (high) normal weight
In lipohypertrophy and lipedema, there is disproportion between the waist and legs (Figure 1, left). Typically, the ankle is the lower end of the increased fatty tissue, the foot is not changed in shape,1,2,6 and often a groove or furrow is observed at the ankle2 (Figure 1, middle).
In obese women
In this case, the disproportion between the waist and legs has been partially lost due to obesity. Typically, the furrows are also found on the thighs and knees or calves. The foot remains without an increase in volume, with the typical furrow at the ankle (Figure 1, right).

Figure 1. Left: Dorsal aspect of a woman with disproportion between a slim waist and high fat deposition in gluteal and thigh region. This could be lipedema or lipohypertrophy. Middle: Calf and ankle of a woman with fat deposition on the calf, respecting ankle and foot. A furrow is found at the ankle. This could be lipedema or lipohypertrophy. Right: Obese woman with furrows on the legs, no fat tissue deposition at the foot. As there is no disproportion, we cannot consider lipohypertrophy. Only if the history demonstrates disproportion in earlier years (before increasing the weight) and there is tenderness on palpation can we consider lipedema.
Images courtesy of © Erika Mendoza.
Palpation of lipedema and lipohypertrophy
In both lipedema and lipohypertrophy without accompanying lymphedema, we do not find any dents when we press into the tissue,2 as we do with lymphedema. The difference between the two lies in the spontaneous pain or pain on palpation, which is pathognomonic for lipedema.1,2,5,6 It is typically symmetrical and can be reduced by compression stockings.1,2,6
What does lipohypertrophy feel like?
The increase in fatty tissue in lipohypertrophy is soft and mobile. The fatty tissue is painless to the touch.2 However, if there is muscle or fascia pain or back-related leg pain, this can be confusing. In case of muscle pain, this appears after “deeper” pressure reaching the fascia with the fingers on palpation. Touching, wobbling, or pressing superficially on the fat layer does not provoke pain.
What does lipedema feel like?
With lipedema, the fatty tissue is more compact on touch (unless the patient has just lost weight). Superficial palpation is immediately painful.1,2 This typical lipedema pain is greatly reduced by wearing compression garments. If there is any doubt, the patient might try support leggings or capri pants to sort out the effect. If support stockings help, the patient might be provided with compression stockings or panties. If there is no relief or the stockings are even bothersome, lipedema can be safely ruled out. The reason for the pain may be orthopedic pain that can be treated otherwise.
How can we tell the difference?
Not all patients with increased fatty tissue on the legs and certain leg pain suffer from lipedema. We therefore need to differentiate between the various possibilities, to find the correct diagnosis but also to give the patient the deserved help against the pain. For example, different types of pain include the following: i) symmetrical pain— probably lipedema (especially if compression helps)1,2,5,6; ii) pain on superficial contact—probably lipedema (especially if compression helps); iii) deep pain to the touch—possible neuromuscular or rheumatological cause, fascial adhesions1; iv) asymmetrical pain that is dependent on posture (more so when standing or sitting) or movement patterns, suggesting an orthopedic, eg, joint condition; and v) asymmetrical pain that is dependent on posture (more so when recumbent), suggesting a spine condition.11
Labeling the patient with the diagnosis “lipedema” often means that no doctor looks for other causes of the pain, leaving the patient with no diagnosis on the real cause of the pain and the needed treatment.
Coexistent obesity and lipedema or lipohypertrophy
The condition lipedema or lipohypertrophy by definition means a higher fat deposition on the extremities. This automatically increases the body weight, even if the rest of the body is slim. Thus, the body mass index (BMI) as a measurement of being overweight can be misleading. Nevertheless, weight is still a tool to help distinguish between obesity and lipedema or lipohypertrophy.1,12
The waist-to-height ratio (WHtR) has been introduced to overcome this problem. The ratio is calculated as follows: waist circumference (in cm) divided by height (in cm). Table I shows the normal and overweight values calculated for women by BMI and WHtR.1,12
Edema in lipedema and lipohypertrophy
Patients with lipedema or lipohypertrophy may develop coexisting edema, perhaps at the end of the day, especially if there are coexisting conditions, such as obesity, sedentarism, and intake of edema-promoting drugs.1 Patients report swelling of the ankles, calves, or feet in the evening. They may show pitting edema on palpation in the evening. If clinically not visible, the feeling of bursting of the ankles the patients describe can be visualized in ultrasound as lines of water between the fatty layer and the bone or the muscle fascia next to the ankle. This is always an indication to wear knee-long compression stockings to treat and prevent this condition. This edema is not pathognomonic for lipedema but can coexist with the disease.1,2
Thigh swelling in lipedema
Some women affected by lipedema describe a subjective perception of turgidity and swelling in the thighs that increases during the course of the day. A small pilot study was run to confirm if the thighs actually swell during the day in lipedema or not.13
In an in-hospital setting, 14 female patients with a confirmed diagnosis of lipedema and who reported suffering from swelling of the thigh throughout the day would have their thigh circumferences measured by the same person in the morning and the evening, all on the same day. They remained without compression. The investigation took place on a Saturday, with no treatments scheduled apart from a walk. Ten control, female patients, adjusted for BMI and hospitalized for arm lymphedema after breast cancer, underwent the same measurements on the same day.
The mean circumferential change during the day ranged from 0 to 0.64 cm for the women with lipedema and from 0.3 to 0.8 cm for the subjects in the control group, none of which were large amounts. No statistically significant differences were found.
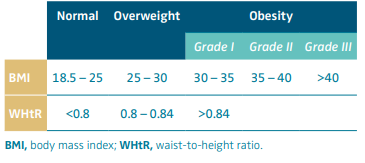
Table I. Values indicating normal weight, overweight, and obesity measured by BMI (body mass index) or WHtR (waist-to-height ratio).
Based on reference 1: Faerber G. S2k-Leitlinie Lipödem. AWMF-Registernummer 037-012. https://register.awmf.org/de/leitlinien/
detail/037-012 (English translation expected online at the same web
address August 2024).
Lymphedema
Visual inspection of lymphedema
Lymphedema in the legs can start in the thigh (often after cancer surgery in the pelvis, Figure 2, left), in the feet (Figure 2, middle), or affect all parts of one or both legs (Figure 2, right). Particularly with lymphedema of the thigh, you can see the imprint of the edge of the seat after standing up (Figure 2, right).
Lymphedema often also affects the feet. The forefoot then bulges, and thickening of the toes can be observed, which develop the appearance of “boxes” with grooves at the base of the toes (“box toes”) (Figure 3, left). Particularly in summer, when compression is often omitted due to the heat, small blisters may appear on the skin, with clear fluid oozing out (Figure 3, middle). Depending on the extent of the lymphedema, the skin can turn reddish-brown (Grade III) (Figure 3, middle and right) and even lead to an ulceration. In advanced cases, but also with additional poor skin care, wart-like skin changes with scaling occur (Figure 3, right).9
Palpation of lymphedema
Lymphedema feels like cake batter or Plasticine; if you press into the tissue with your finger (Figure 4, left), a dent remains, which only fills up again after a few minutes9 (Figure 4, right). Depending on the degree of lymphedema, the accumulation of protein in the tissue increases, then the texture changes from soft (Figure 5, left and center) to hard or “stony” (Figure 5, right) and only leaves a slight impression after half a minute of hard pressure.9

Figure 2. Left: Lymphedema of the left leg after iliofemoral tumor (sarcoma) with surgery and radiation. The leg difference is caused by the lymphedema deposition in the subcutaneous tissue without treatment over a long time. Middle: Lymphedema in a woman with terminal cervix cancer after Wertheim surgery and radiation. The patient is underweight (43 kg) and still has lymphedema on the legs with box toes. Right: An 82-year-old man with lymphedema after prostate-carcinoma with surgery and radiation. He usually sits and is no longer able to move. Lymphedema accumulates in the dependent areas and has a high plasticity. After the patient sits 3 minutes on the examination couch, a depression in the edema is apparent.
Images courtesy of © Erika Mendoza.

Figure 3. Left: Typical changes at the toes of lymphedema patients: furrows at the base of the toes, filling with lymphedema, so that the form of the toe is no longer round, but like a box. It is impossible to take a skin fold at the toes (Stemmer sign). Middle: After a longer period of persistence of the lymphedema, the skin develops sclerosis with discoloration and atrophy of the fatty tissue. Without compression, the lymphatic fluid will ooze out of small blisters on the skin. Right: Lymphedema at an advanced stage, with furrows and caused by poor skin care; wart-like skin changes with scaling.
Images courtesy of © Erika Mendoza.

Figure 4. Testing for lymphedema: compressing with a finger (left), a depression develops that stays throughout a period of minutes (right). In this case, with early lymphedema, the tissue is soft on touch.
Images courtesy of © Erika Mendoza.
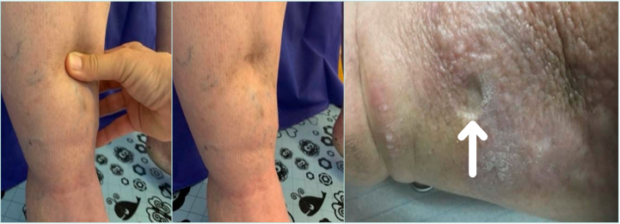
Figure 5. Left and center: Lymphedema in Grade II, it takes more force to provoke the depression and it stays longer. Right: In very advanced protein-rich lymphedema, it takes some minutes to pinch a finger cusp inside the tissue—the dot provoked (see arrow) stays for hours.
Images courtesy of © Erika Mendoza.
Coexistence of lymphedema and lipohypertrophy or lipedema
If women with lipedema or lipohypertrophy develop massive obesity, “obesity-related” lymphedema can also occur. Figure 6 shows a case of lipedema with bulge formation and furrows, obesity, and obesity-related lymphedema with box toes at the feet on the same leg. We know that this is lipedema and not lipohypertrophy, as she has pictures from her youth showing disproportion between abdomen and legs and she reports that she has always suffered from pain. She has worn compression stockings regularly since she was 18 years old. Prior to this image, the patient had lost 30 kg, dropping from 180 kg to 150 kg, to be admitted for a knee-joint surgery.
Some people call this “lipo-lymphedema,” which is an inappropriate term, as the lymphedema is not secondary to the lipedema, but to the obesity. Lymphedema and lipedema are completely different clinical entities.14 An overview of characteristics for the 4 conditions is given in Table II.
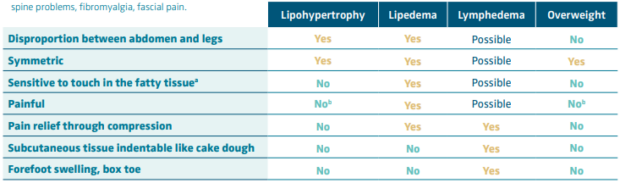
Table II. Overview of characteristics from lipedema, lipohypertrophy, lymphedema, and obesity. aPlease distinguish between pain in the fatty tissue or pain on deep touch with compression of the fascia or muscular tissue, often painful in sedentary persons. bUnless there are other causes, such as muscle pain, lumbar spine problems, fibromyalgia, fascial pain.
Leg changes with obesity
Some patients have generalized obesity. The furrows in the tissue are caused by the excess weight; it is present all over the body and does not cause pain to the touch.1,2 This is obesity and not another disease entity. However, this obesity will often lead to lymphedema (see Figure 6). The degree of lymphedema reduces or the condition even disappears after weight reduction.14

Figure 6. Women with lipedema with “dewlaps” (ie, excessive, almost hanging fatty tissue) and furrows, in a patient after losing 30 kg with additional lymphedema. Note the reddish discoloration of the very bulging tissue in front of the shin, here a “kneadable” consistency when touched, with involvement of the forefoot with furrows between the toes and the back of the foot.
Images courtesy of © Erika Mendoza.
Summary
Lipedema, lymphedema, lipohypertrophy, and obesity are 4 conditions with similar manifestations, making differential diagnosis challenging. However, differentiation can be made easier if basic concepts are clear.
Diagnosis is based on medical history and physical exam, visual inspection, and palpation being the key items. An improvement of the definitions of these entities including the renaming of lipedema disease to avoid conception of edema associated with lipedema is needed. Educational activities promoting these fundamental keystones among health care workers and the general population will improve diagnosis, and consequently management.

CORRESPONDING AUTHOR
Erika Mendoza, PhD
Speckenstr. 10, 31515 Wunstorf,
00 49 5031 912781, Germany
EMAIL: erika.mendoza@t-online.de
References
1. Faerber G. S2k-Leitlinie Lipödem. AWMF Registernummer 037-012. https://register. awmf.org/de/leitlinien/detail/037-012 (English translation expected online at the same web address August 2024).
2. Bertsch T, Erbacher G, Elwell R, Partsch H. Lipoedema: a paradigm shift and consensus. J Wound Care. 2020;29(Sup11b):1-52.
3. Bertsch T, Erbacher G. Lipoedema – myths and facts Part 2. Phlebologie. 2018;47(3):120-126.
4. Faerber G. Obesity and chronic inflammation in phlebological and lymphatic diseases. Phlebologie. 2018;47:55-65.
5. Forner-Cordero I, Pérez-Pomares MV, Forner A, Ponce-Garrido AB, Muñoz-Langa J. Prevalence of clinical manifestations and orthopedic alterations in patients with lipedema: a prospective cohort study. Lymphology. 2021;54:170-181.
6. Forner-Cordero I, Forner-Cordero A, Szolnoky G. Update in the management of lipedema. Int Angiol. 2021;40(4):345-357.
7. Allen E, Hines E. Lipedema of the legs: a syndrome characterized by fat legs and orthostatic edema. Proc Staff Mayo Clin. 1940;15:184-187.
8. Grigoriadis D, Sackey E, Riches K, et al. Investigation of clinical characteristics and genome associations in the ‘UK Lipoedema’ cohort. PLoS One. 2022;17(10):e0274867.
9. International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema: 2013 Consensus Document of the International Society of Lymphology. Lymphology. 2013;46(1):1-11.
10. Rockson SG. Advances in Lymphedema. Circ Res. 2021;128(12):2003-2016.
11. Mendoza E. Differential diagnosis of leg pain in phlebology. Phlebologie. 2019;48:366-372.
12. Brenner E, Forner-Cordero I, Faerber G, Rapprich S, Cornely M. Body mass index vs. waist-to- height-ratio in patients with lipohyperplasia dolorosa (vulgo lipedema). J Dtsch Dermatol Ges. 2023;21(10):1179- 1185.
13. Erbacher G, Mendoza E, Bertsch T. Thigh swelling in patients with lipedema – subjective perception versus objective examination. Vasa. 2022;51(6):386-388.
14. Bertsch T. Obesity-related lymphoedema – underestimated and undertreated. Phlebologie. 2018;47:75-83.
