History of venous surgery (1)
This is the first of the 3 chapters that make up a “History of Venous Surgery”. These chapters will be published consecutively in Phlebolymphology.
Michel PERRIN
Vascular surgery,
Lyon, France
INTRODUCTION
Before discussing the history of venous surgery, we thought it would be desirable to provide a short semantic and etymological review to clarify or define certain terms that we will use throughout this historical review.
SEMANTIC REVIEW
Etymologically the word surgery can be defined as the practice of a treatment by using one’s hands. It derives from the Greek χειρουργια (kheirourgia) χειρ (kheir) [hands] and εργον (ergon) [work]. In modern language, the word surgery is used to denote any therapeutic procedure which involves one or more cutaneous incisions, or in other words, open surgery.
In this review, we will use the older definition, ie, any therapeutic intervention consisting of a manual procedure which includes all endovascular treatments that can be performed by venipuncture. Currently, such techniques are increasingly used.
To study the chronology of venous surgery, a few other terms should be explained:
Chronic venous disease or chronic venous disorders refer to all venous diseases of the lower limbs which progress gradually and slowly; they are the opposite of acute venous disease which is the sudden occurrence of a disorder affecting the veins. Traditionally, as we have specified, chronic venous disorders only concern the lower limbs, while the term acute venous disease can be used for all veins, whatever their location.
Varicose veins. These venous disorders most commonly affect the lower limb, commonly and inappropriately referred to as the “leg”, even though anatomically, the leg is the region extending from the knee to the foot. Varicose veins of the lower limbs can be described as a visible dilatation of the superficial veins which most often have a tortuous appearance. Their function is altered insofar as they have lost their ability to return venous blood effectively to the heart. Varicose veins are classified as a chronic venous disease.
A thrombosis is the occurrence of a blood clot in the lumen of a vein; this term should be used instead of “phlebitis”*, which etymologically means inflammation of a vein. The terms paraphlebitis and periphlebitis, still sometimes used, should be banned because they do not correspond to any defined venous disease.
A thrombosis is an acute venous disease; it can affect the three venous systems of the lower limb, either as an isolated event or in combination, but it is deep vein thrombosis which is the most harmful. Such thrombosis quite often produces late-onset complications, in particular when it occurs in a deep vein of the lower limb, and then we refer to it as postthrombotic syndrome. Unlike acute thrombosis, postthrombotic syndrome is a chronic venous disease because, like a varicose vein, it progresses and worsens.
* Phlebitis. At that time and unfortunately even today, the difference between phlebitis—an inflammation of the walls of the vein—and venous thrombosis, is not always respected. It is true that the two events are always associated with deep veins but in this case the term deep vein thrombosis is always used, while in the superficial veins they can be separate (superficial phlebitis or “veinitis”) or combined (superficial thrombophlebitis).
REVIEW OF ANATOMY AND PATHOLOGY
In the lower limb, veins are distributed into three systems.
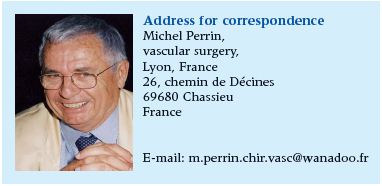
• The superficial venous system (Figure 1), divided into two networks
– Two collecting veins, the saphenous veins: the great saphenous vein (GSV) and the small saphenous vein, which are located in the superficial fascia.
– The non-saphenous veins lie outside of the fascia. They drain blood from the superficial tissues into the saphenous veins; the term “collateral vein” should no longer be used to denote them, the most appropriate term is tributary vein. Therefore, there are tributary veins of the GSV and of the small saphenous vein.
The term varicose veins is reserved for abnormal veins in the superficial venous network.
• The deep venous system.
1 great saphenous vein; 2-5. tributaries of the saphenous veins; 6.
small saphenous vein; 7 vein anastomosing with the great and
small saphenous veins
Source: Perrin M. Affections veineuses chroniques des membres
inférieurs. Généralités. Rappel anatomique et
physiologique. EMC (Elsevier SAS, Paris), Techniques
chirurgicales – Chirurgie vasculaire, 43-160, 2006.
As its name suggests, this system is located in the deep tissues in the sub-fascia compartment and it drains 80 to 90% of venous blood. The two saphenous veins empty into the deep venous system. The GSV empties into the common femoral vein and its distal segment is called the saphenofemoral junction. The small saphenous vein most commonly ends in the popliteal vein and its distal segment is called the saphenopopliteal junction.
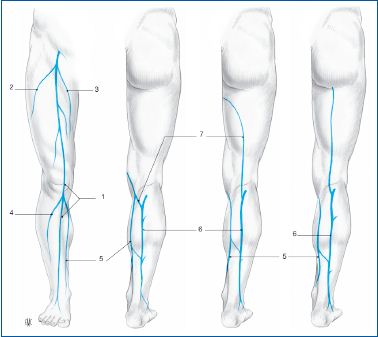
a. Free border of valvular cusp; b. valvular commissure; c. valvular
sinus; d. Implantation of valvular cusp on vein wall.
Source: Perrin M. Affections veineuses chroniques des membres
inférieurs. Généralités. Rappel anatomique et
physiologique. EMC (Elsevier SAS, Paris), Techniques
chirurgicales – Chirurgie vasculaire, 43-160, 2006.
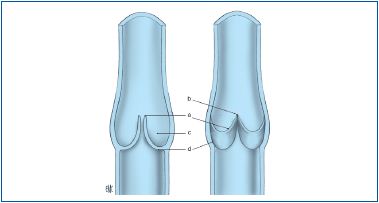
ultrasound appearance
The 2 open cusps are identified in the venous lumen and appear as
2 vertical white lines separated from each other.
Source: Perrin M. Affections veineuses chroniques des membres
inférieurs. Généralités. Rappel anatomique et
physiologique. EMC (Elsevier SAS, Paris), Techniques
chirurgicales – Chirurgie vasculaire, 43-160, 2006.
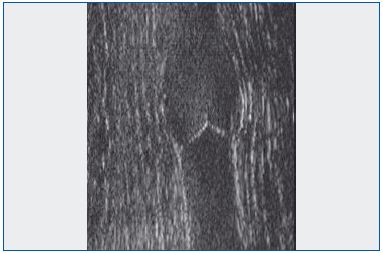
ultrasound appearance
The 2 valvular cusps whose free borders are in contact in the
venous lumen are identified by a circumflex
Source: Perrin M. Affections veineuses chroniques des membres
inférieurs. Généralités. Rappel anatomique et
physiologique. EMC (Elsevier SAS, Paris), Techniques
chirurgicales – Chirurgie vasculaire, 43-160, 2006.
• The perforating vein system.
These are veins which anastomose with the deep and superficial venous systems, in addition to the saphenous junctions.
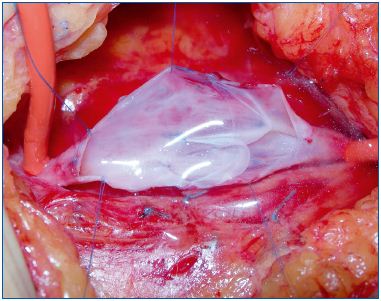
Courtesy; Maleti MD.
The valvular apparatus The lower limb veins below the inguinal ligament contain valves in their lumen and along their entire length (Figures 2a, 2b, 2c, 2d) which allow blood flow only from the periphery to the heart. A valvular lesion can be of unknown or poorly identified cause (idiopathic), as is the case in so-called primary varicose veins or in primary deep vein insufficiency. Valvular lesions or abnormalities can either have a known cause (postthrombotic) or, in rare instances, be congenital.
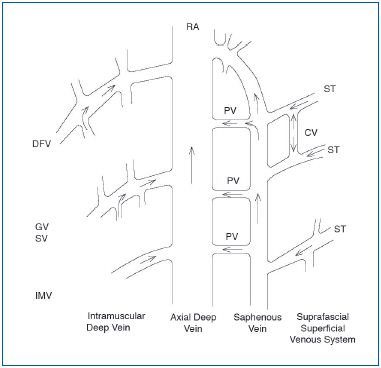
IMV: intramuscular vein; PV: perforating vein; CV: communicating
vein; ST: saphenous tributary.
REVIEW OF PHYSIOLOGY
In the lower limb, blood flows from the superficial veins into the deep veins at the saphenous junctions and through the perforator veins (Figure 3). The deep veins return blood to the heart via the iliac veins, and then the inferior vena cava. The latter ends in the right atrium after crossing through the abdomen and the thorax.
HISTORY OF VENOUS SURGERY
It might seem reasonable that venous surgery only began after scientific knowledge had been acquired on the anatomy and physiology of the veins and on their pathology and pathophysiology. There is, in fact, no truth to this, but this is not specific to veins. During each era “specialists” were persuaded that they had knowledge which in fact proved erroneous and unfounded as advances were gradually made in this field. In the 17th century, Molière had a premonition of this event by making fun of the practice of bleeding someone to treat any disease. It is possible, or even likely, that our current knowledge of venous disease and its treatment with surgery will be called into question in future decades.
For a long time, venous surgery was limited to varicose veins.
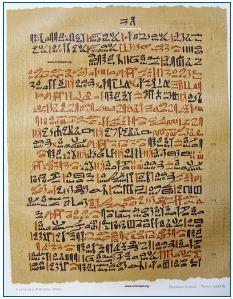
Ancient Egypt
The Ebers Papyrus (27th Pharaonic dynasty, 1580-1320 BC) clearly contraindicated surgery for varicose veins:
“Instruction concerning swelling of blood vessels. If thou examine a swollen blood vessel under the skin of a limb and its aspect increases, becomes sinuous and serpentine, like something swollen with air, then thou will say concerning it, it is a swollen blood vessel—Thou shall not touch something like this” (Figure 4).
The Greco-Roman era
Hippocrates, born in Kos (Greece), was also relatively opposed to surgery for varicose veins. At most, he recommended making punctures or tiny incisions in them once, supplemented by compression, but emphasized that the occurrence of an ulcer could be related to the incisions.
Aulus Cornelius Celsus (Rome, flourished Ist century AD) was probably one of the first to operate on varicose veins, but it is not known with certainty if he was a doctor. He performed avulsion of varicose veins with a hook—today this technique is called phlebectomy by mini-incision. He gave us a precise description: “Make an incision of the skin covering a varicose vein, spread apart the edge of the wound with a small hook and use a scalpel to detach the varicose vein from the surrounding parts, taking care not to injure them. After it has been detached, a small blunt hook is placed below it, always leaving a 4-finger interval between the incisions, and the same operation is continued on the vein. It is easy ascertain its direction by the hook method. Thus, after these varicose veins have been detached, they are removed with the hook, next to which they are cut: then the nearest hook is passed, with which the vein is removed in the same manner and is again cut at this place. Thus, after removing all varicose veins from the leg, the edges of the wound are brought close together by applying an agglutinating plaster.”
Certainly, the current technique of phlebectomy is slightly different, but the principle is the same, it involves closer and closer excision of the varicose vein. What did definitely change is the pain experienced by the patient during this procedure. In fact, Caius Marius, the Roman tyrant who died in 86 BC, was very probably given a red wine “anesthetic” as pre-medication as was the custom at the time before an operation. He refused to be operated on the other side and declared that the “treatment was worse than the disease”. Tumescent local anesthesia, currently used in surgery for varicose veins, is as effective as it is painless.
A very complete Byzantine document was written a few centuries later by Oribasius of Pergamum (325-395?). Varicose vein surgery fills three chapters of his surgery book on this topic and some of its recommendations are still relevant:
1. Resection of veins is preferable to ligation, which can cause new varicose veins.
2. Shave and wash the limb (with hot water) before operating on it.
3. While the limb is still warm, mark the varicose veins on the skin with the patient in standing position.
4. Resect the veins of the leg before those of the thigh.
5. Remove blood clots (hematoma) by pressure on the operated limb.
Aetius of Amida (Mesopotamia 502-575?) appears to be the first to have proposed ligation of varicose veins.
Paul of Egine, also a Greek (607-690?), provided a new approach by combining phlebectomy and ligation in treatment of the varicose GSV.
The Arabs
The most famous surgeon of his time was an Andalusian from Córdoba (930-1013?) Abu-Al-Qasim Khalaf Ibn’Abbas Al-Zahrawi, and thankfully posterity hasretained only the last part of his name, who described stripping of the great saphenous vein in an exceptionally detailed manner.
The Middle Ages and the Renaissance
The Frenchman Guy de Chauliac (1298-1368), probably the only doctor to have treated four popes in Avignon, France, proposed a classification system of cutaneous ulcers based on their appearance (Figures 5 a, b, c, d) in his 4-volume treatise on surgery. He classified them as “clean and healthy, virulent and corrosive, sordid and rotten, deep and cavernous.” The most common venous etiology in the lower limb would only be established much later, but the illustrious “surgeon” from Montpellier proposed treatment by cauterization of both the ulcer and the varicose veins. Ambroise Paré, a French anatomist and surgeon (1510-1590), recommended exactly the same treatment 200 years later.

Figure 5b. Medial venous ulcer at the gaiter area with a necrotic zone.
Figure 5c. Large medial venous ulcer at the gaiter area.
Figure 5d. Lateral venous ulcer surrounded by lipodermatosclerosis and eczematous dermatitis.
The 17th and 18th centuries
Although the Englishman William Harvey was the first to correctly describe the physiology of the venous circulation in 1628 in a work entitled “Exercitatio Anatomica de Motu Cordis et Sanguini in Animalibus” (Figures 6 a, b), the leadership in surgery remained in continental Europe in the 17th century with the Frenchmen Pierre Dionis (1643-1718) surgeon to the Royal Family, and a contemporary of Molière and of Jean-Louis Petit (1674-1750), who was a member of theRoyal Academy of Surgery under Louis XV. Both Dionis and Petit advocated surgical treatment of varicose veins with no special innovative technique, although Dionis expressed the reservation that “ligation of a vein can be cruel and painful and have unpleasant effects.”
identifying the role played by valves in the venous circulation.
with plunger and hollow needles.
Johannes Schultheiss, a German surgeon whose Latin name was Scultetus (1595-1645), developed his own hooks to perform phlebectomy.
In the 18th century, leadership in surgery crossed the English channel. John Hunter (1728-1793) a Scot, took up a range of topics, both in medicine and in surgery. In vascular surgery, in particular, he is known for having performed surgical treatment on an arterial aneurysm of the popliteal artery, but he was also interested in venous disorders and described a pulmonary embolism and differentiated septic phlebitis from traumatic phlebitis.
The 19th century
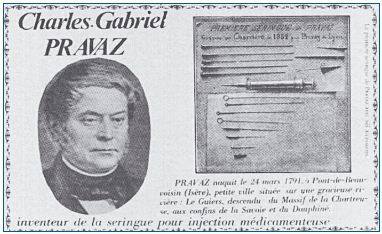
The treatment of varicose veins took a new direction with the development of sclerotherapy. The term sclerotherapy refers to injection of a sclerosing product into the lumen of a vein which gradually results in destruction of the vein. Some will object that this method is not surgery. This is incorrect if we use the definition given in the introduction, all the more so since the precursor of this method, the Frenchman Charles Gabriel Pravaz (1791-1853), although a graduate of the elite École Polytechnique, was also a surgeon. In 1841, Pravaz designed and made a syringe out of silver, 3 cm long and 5 mm in diameter, intended for injection of ferric perchloride into an arterial aneurysm, for coagulant purposes. The plunger of the syringe descended by tightening of a screw, thus making it possible to control the quantity of substance injected. He then fitted a hollow needle on the end of this syringe (Figure 7) which allowed injection of the syringe contents into the vascular lumen. In fact, it was the surgeons of Lyon who lived at the same time as Pravaz, and in particular Joseph Pierre Pétrequin (1809-76), surgeon in chief of the Hôtel Dieu hospital, who deserve the credit for having applied this method to the treatment of varicose veins. But the occurrence of serious adverse events discredited this method. We can judge for ourselves: following 411 injections, Weinlechner in Germany reported 18 cases of localized gangrene.
Surgery involving removal of varicose veins saw little technical change in the 19th century. In 1884, the German Otto Wilhelm Madelung proposed making an incision along the entire length of the vein to resect it, but this was not cosmetically acceptable and was responsible for an almost 1% incidence of fatal pulmonary embolism.
In 1890, the German Friedrich Trendelenburg limited his intervention to ligation of the GSV a few centimeters from its end in patients with saphenofemoral junction reflux associated with one or more incompetent terminal valves of the GSV. It is of interest to note the following: – Such ligation of the GSV at a distance from its point of emptying into the deep vein left in place a segment of the GSV which drains a large number of tributaries above an incompetent valve (Figure 8). Thus, theoretically the reflux was not eliminated and it worsened or produced a dilatation and a reflux of the tributaries of the GSV since the filling reservoir represented by the trunk of the GSV was eliminated by its removal. In practice, this change was not constant.
– Moreover, Trendelenburg performed this procedure so quickly that no anesthesia was necessary …
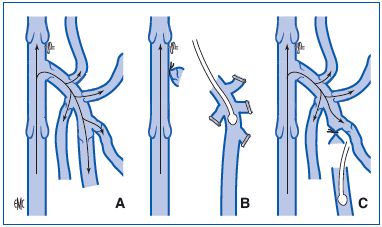
Incompetent terminal valve of the great saphenous vein responsible
for femoro-saphenous reflux during the Valsalva maneuver.
B. Ligation of the end of the great saphenous vein at a distance
from where it empties into the deep vein in the same patient. The
stump of the arch left in place allows persistence of reflux through
the incompetent terminal valve of the great saphenous vein which
will dilate the tributaries of the great saphenous vein.
Source: Perrin M. Insuffisance veineuse superficielle: notions
fondamentales. EMC (Elsevier Masson SAS, Paris),
Techniques chirurgicales – Chirurgie vasculaire, 43-161-A, 2007.
In 1896 Moore, an Australian, recommended ligation of the GSV at the level where it empties into the deep vein.